PCOS and Insulin – When Diet Is Not Enough
May 4, 2019
This post is written by supplement company that produces high quality products: Designs for Health. I recommend and personally use a few of their supplements for PCOS: Sensitol and N-Acetyl Cysteine. I also love their Whole Body Collagen. I can guide you in appopriate use of supplements and offer my patients a significant discounts on professional grade products, including those from Designs for Health. My comments are in italics.
Polycystic ovary syndrome (PCOS) is one of the most prevalent conditions affecting women’s reproductive health. As practitioners, we are well aware that the body’s hormone network is highly complex and interwoven with many other metabolic pathways, so PCOS is not just a hormonal condition, but an endocrine disorder, as well. Characterized by polycystic ovaries, chronic anovulation, and hyperandrogenism, the leading symptoms of PCOS include irregular menstrual cycles, hirsutism, acne and infertility.
Insulin resistance, compensatory hyperinsulinemia, and reduced insulin clearance are primary metabolic abnormalities associated with the development of PCOS. Compared to age and BMI-matched controls with prediabetes (but no hyperandrogenism and ovulatory disorders), those with PCOS have significantly higher levels of insulin 2 hours following an oral glucose tolerance test and a lower metabolic clearance rate of insulin (MCRI), but a similar degree of insulin sensitivity. Therefore, insulin clearance may be a factor that distinguishes the endocrine dysfunction of PCOS from that of type 2 diabetes.
Similarly, obesity is often a characteristic associated with PCOS and has led many to believe that type 2 diabetes was an underlying cause of PCOS; however, rising numbers of lean women are also presenting with PCOS and confusing the theory that insulin resistance in PCOS is a result of obesity. In a meta-analysis study
comparing insulin resistance and sensitivity among obese or non-obese women with PCOS, and obese or non-obese healthy controls, it was found that obesity alone did not have a statistically significant effect on insulin resistance and sensitivity (although obesity certainly increased insulin resistance), but the presence of PCOS had a greater effect on insulin resistance than was caused by obesity alone.
Another study
seeking to understand how insulin resistance in PCOS is independent of obesity compared insulin resistance and β cell function in lean PCOS patients with obese PCOS controls. Interestingly, the lean PCOS patients had a similar β cell function and insulin resistance as compared to controls. Additionally, fasting c-peptide and its ratio to glucose were significantly higher in lean patients compared to controls. Together, these results indicate that the insulin metabolism of PCOS is, again, independent of obesity.
Although insulin-sensitizing pharmaceuticals are traditional recommendations for addressing the hyperinsulinemia associated with PCOS, more conservative and natural approaches often focus on a low-sugar, Paleolithic or Ketogenic styles to control blood sugar and insulin levels. While these diets most certainly play a crucial role in optimizing the health of the whole body and balancing blood sugar levels, they are most effective in those who also experience obesity coupled with PCOS. As weight is better managed by rebalancing blood sugar, insulin is better regulated. However, in the lean population with PCOS (and even in many of the obese patients with severe cases of PCOS), a low-sugar diet alone is not enough to address the insulin complications.
Inositol
Various botanicals and nutraceuticals are helpful in improving insulin resistance and sensitivity when the diet is not enough. In a randomized controlled trial, 50 women with PCOS, insulin resistance, and hyperinsulinemia were given either 4 g per day of myo-inositol or 1500 mg per day of metformin, the commonly prescribed insulin-sensitizing drug. After 6 months, both groups experienced improvement in insulin sensitivity, indicating inositol may be just as effective as metformin for women with PCOS. This is an active ingredient in Sensitol.
Berberine
Berberine is an isoquinoline derivative alkaloid extracted from various Chinese medicinal herbs that has also been used as an insulin sensitizer. In a randomized controlled
trial of 89 women with PCOS and insulin resistance, berberine treatment was compared with metformin for 3 months. It was found that berberine effectively improved body composition, lipid levels (which are often imbalanced in PCOS due to sugar dysregulation), sex hormone-binding globulin, fasting plasma glucose, fasting insulin, and insulin resistance. A meta-analysis and systematic review
confirmed the same conclusion that berberine improves insulin resistance and glucose metabolism similar to metformin.
Cinnamon
Though not compared to metformin, cinnamon powder has also been shown to improve insulin resistance, glucose metabolism, and lipid profiles in women with PCOS. In a randomized double-blind placebo-controlled clinical trial, 80 women with PCOS were given 1.5 grams per day of cinnamon powder capsules for 12 weeks or a placebo. Improvements were noted in fasting insulin and insulin resistance in those taking the cinnamon compared to placebo.
The clinical outcomes of PCOS, including infertility, severe acne, and hirsutism, are often devastating for women. Hormone balance to address hyperandrogenism is most often the focus of treatment, but as an increasing amount of research points to insulin resistance as an equally influential element of PCOS, a focus on insulin sensitizers can’t be ignored. Diet is a great place to start in rebalancing glucose, but it is often not enough. Inositol, berberine, and cinnamon can also provide the support needed to address insulin resistance in these situations.
I personally prefer N-acetyl cysteine over berberine and cinnamon. Other effective nutritional suppements include reishi mushroom, green tea, and spearmint tea.

There is probably nothing that tastes better than a fresh hot French Fry, dusted with salt and dipped in ketchup - YUM! One of my favorite flavors! On the other hand, when I advise clients on "foods" to avoid or totally remove from their usual diet, the number one food on this (relatively short) list to avoid is fried foods. A no-brainer you are thinking - they are high in calories. Okay, yes, high in calories, but is that all that they are high in? Hardly. The also contain several toxic by-products from the repeated high heating of liquid frying oils. By toxic, I mean quite literally toxic to the human body. In fact, if someone has or had cancer, or has a high risk for cancer, I advise them to absolutely restrict their intake of all fried foods, along with other environmental toxins. Take a look at these conclusions made by scientists regarding the consumption of the frying oil present in all fried foods: Investigations have repeatedly demonstrated the heat-promoted generation of very high levels of highly toxic aldehydes in such products (particularly those fried in oils rich in in PUFAs - such as soybean and canola oil). , These findings have been available to the scientific, food and public health research communities since 1994. Used frying oils collected from domestic kitchens, fast-food retail outlets and restaurants, have confirmed the generation of these aldehydes at high concentrations during ‘on-site’ frying practices. Of critical importance to their public health risks as food-borne toxins , typical aldehydes produced during standard frying practices are absorbed from the gut into the circulation where they cause damage to cells, tissues, and essential organs. These toxic aldehydes (and other by-products) cause cellular stresses, and lead to adverse health effects on critical metabolic pathways - notably including on energy metabolism. Even with minimal or no heating, most of the oils used do not contain enough vitamin E to protect the highly oxidizable polyunsaturated fatty acids (PUFAs) they are high in. A Duke study of 4,000 children showed that potato chips, fried chicken and fish, and French fries were the top obesity-promoting foods. These foods also exert mutagenic (gene altering) and carcinogenic properties, teratogenic actions (which cause birth defects) and other striking pro-inflammatory effects. Finally, if you are trying to get pregnant, neither you or your partner should be eating fried foods more than once a week as adverse effects on sperm quality are well documented. We continue to learn more about the effects on female fertility, but there is a connection to oxidative stress, which is increased by consuming fried foods. These damaged oils stay in our bodies for up to 7 years!!!! With so many delicious foods available to eat in and out of the house, why endanger your health or fertility by eating fried foods? I can help guide you to better choices, please call me! Extra notes: Note I said one of my favorite "flavors" not foods. Because of this knowledge, I rarely eat fried foods, with the exception of a couple of handfuls of tortilla chips when I eat at Mexican restaurants, along with the occasional fried oyster or shrimp appetizer for my birthday or my husband's birthday! Great short video on these dangers: https://www.theepochtimes.com/epochtv/are-vegetable-oils-killing-us-we-swapped-them-in-for-animal-fats-50-years-ago-5391966?utm_source=Morningbrief&src_src=Morningbrief&utm_campaign=mb-2023-07-13&src_cmp=mb-2023-07-13&utm_medium=email For more insights to this widespread dietary problem, here are two great blogs: https://www.alexfergus.com/blog/pufa-s-the-worst-thing-for-your-health-that-you-eat-everyday https://rustonsboneyard.com/whats-the-problem-with-vegetable-oil/ Dr. Perlmutter explains the mechanism of action behind the inflammatory effects of industrial seed oils: https://youtube.com/clip/UgkxePnsNRCUpqfH5MrWRNiHiiqwpQZdEY_o?si=JjXAp8xjlHg7x-Q8 Don't go to Chick-Fil-A more than once a week (if that): https://www.upi.com/Health_News/2019/01/24/Frequent-fried-food-increases-risk-for-obesity-heart-disease-death/4231548336486/ Your genes may be inolved as well: https://www.sciencedaily.com/releases/2014/03/140318190027.htm "Oxidative stress (OS) has been identified to play a key role in the pathogenesis of subfertility in both males and females. The adverse effects of OS on sperm quality and functions have been well documented. In females, on the other hand, the impact of OS on oocytes and reproductive functions remains unclear. This imbalance between pro-oxidants and antioxidants can lead to a number of reproductive diseases such as endometriosis, polycystic ovary syndrome (PCOS), and unexplained infertility. Pregnancy complications such as spontaneous abortion, recurrent pregnancy loss, and preeclampsia, can also develop in response to OS. Studies have shown that extremes of body weight and lifestyle factors such as cigarette smoking, alcohol use, and recreational drug use can promote excess free radical production, which could affect fertility. Exposures to environmental pollutants are of increasing concern, as they too have been found to trigger oxidative states, possibly contributing to female infertility." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527168/ There are ways to make fried foods more safe and less prone to causing oxidative stress in the body, but you cannot really be sure if the restaurant etc. where you purchase food is utilizing the best practices: https://www.researchgate.net/publication/268408525_Nonnutrient_Antioxidants_and_Stability_of_Frying_Oils Toxic aldehyde generation in and food uptake from culinary oils during frying practices: nature.com/articles/s41598-019-39767-1 The USDA recommends that people consume more liquid vegetable oils to get sufficient vitamin E, but this is clearly not the way to do it. Better to eat fresh nuts and seeds, whole grains, dark leafy greens, pastured eggs, and avocados, and supplement as needed with a mixed vitamin E, such as Jarrow Famil-E: https://academic.oup.com/jn/article-abstract/81/4/335/4779307?redirectedFrom=fulltext

Collagen protein from the very start. While clearly beneficial in our senior years, there is a very different stage of life when collagen protein intake is equally if not even more important. That time is during fetal development. [i] Even if you are well past your child-bearing years, please read on as you may be able to share this helpful information with expectant parents. Many women who I help come in with hormonal problems, infertility, or pregnancy complicated by obesity or poor blood sugar control. The women I don’t see anywhere near as often are those that do not experience problems conceiving or carrying a baby to term. This is a real shame because all women can benefit from a thorough review of their diet by a knowledgeable dietitian or nutritionist, before, during, and after pregnancy. Whether pregnant or trying to conceive, my patients consistently tell me how valuable the information I shared with them was and how glad they were to have met with me. In the words of one mother-to-be, “I didn’t know what I didn’t know.” Unfortunately, many women continue to have gaps in their prenatal nutrition despite following the recommended dietary guidelines and receiving the best obstetrical care. Could these gaps lead to problems for a woman or her baby? Based on the growing body of research in reproductive nutrition, the potential is there. [1] My goal is to see all women be fully nourished during the critical life stages of pregnancy and lactation. In my practice, one of the most frequent recommendations I make to pregnant patients is that they consume more collagen protein. They are surprised to learn that daily servings of skin-on organic chicken, gelatin dishes, and soups made with bone broth are important parts of their prenatal diet. And I have yet to meet with an expectant mother that was already in the habit of eating these nourishing foods prior to our first appointment. One of the main reasons collagen protein appears to be essential during pregnancy is, once again, that little amino acid glycine. According to nutritional scientists, “the shortage of glycine may become serious in conditions such as pregnancy.” [ii] What might “serious” mean for a pregnant woman and her baby? Pregnancy creates a higher demand for glycine due to the increased collagen and elastin synthesis taking place in the expanding uterus and stretching skin. As a result, glycine may become a limiting factor for protein synthesis in the developing fetus. Without enough available glycine, there is the possibility that fetal growth will be restricted, albeit to an unknown extent. Additionally, in studies on pregnant rats, glycine supplementation reversed the high blood pressure and the blood vessel dysfunction that occurred when they were fed lower protein diets. [iii] These findings point to an important (pivotal per authors) role for dietary glycine in the adaptations required during pregnancy to support healthy maternal circulation. Recall from chapter 3 that some scientists consider glycine to be one of the conditionally-essential amino acids because the human body cannot synthesize enough glycine to meet more than its most basic survival needs. There are numerous health benefits to consuming sufficient quantities of glycine through diet, 10 grams per day appears to be about optimal. [iv] And while 10 grams may be sufficient for almost every healthy adult, it is almost certain that a moderately higher amount would be beneficial during pregnancy, especially during the last two trimesters when the most rapid growth occurs. To better understand the role of glycine, we need to look at it in the context of the overall diet. It is generally recommended that a woman consume an additional 25 grams of protein per day during the second and third trimesters of pregnancy, or a total of 71 grams protein per day. A lot more protein is not advisable. High protein diets that exceed 20% of calories from protein can impair fetal growth, according to a 2013 review of the research. [v] [2] And an excess of the amino acid methionine relative to glycine is not optimal either. Too much methionine not only increases the need for glycine but may lead to other undesirable effects on the child’s long-term physiology. [vi] Where would an excess of methionine come from? From high protein diets that are often thought of as healthy, and especially ones with predominantly lean muscle protein, like chicken breast and lean meat. So whether it is the total amount of protein or methionine, or the ratio of methionine to glycine consumed, it is important to make sure that the sources of protein are balanced, avoiding too little as well as too much. Nutritionists often referred to this as the “Goldilocks Principle” and it can be applied to almost any nutrient, supplement, or food that we consume. Of course collagen protein, although an excellent source of glycine and other amino acids, is just one component of a nourishing diet! When I am asked what the perfect meal for a pregnant woman is, I answer: a great homemade soup made with collagen-rich bone broth, one to two ounces of meat, poultry, organ meat, or safe seafood, one ounce of soft-cooked tendons such as in the traditional Vietnamese dish Pho, plenty of fresh leafy greens, a small potato or sweet potato, a half-cup of a favorite type of legume, a whole egg or even better two egg yolks, a bit of seaweed rich in iodine, and a handful of cilantro or other green herbs. On the side would be a fermented vegetable like sauerkraut. This would be accompanied by a good source of calcium such as a grass-fed cheese or yogurt, along with a fresh fruit for dessert, topped off by a little sunshine for vitamin D! Come to think of it, this is a perfect meal for just about anybody, at any time! Recovery after delivery. Collagen protein consumed throughout pregnancy could have further benefits after delivery. We already know that pregnant women need more collagen protein because a high proportion of them have been shown to have a glycine insufficiency. [vii] It has also been shown that with each pregnancy, the collagen and elastin content of a women’s uterus increases. [viii] Stretch marks happen when a women’s belly expands faster than her skin can keep up with, causing the collagen and elastin fibers in your skin to break. Because collagen protein has been shown to increase the elasticity of the skin, it just might minimize the appearance of those annoying stretch marks. Other than not gaining excessive weight during pregnancy, medical experts don’t know how to prevent stretch marks. Collagen protein in the context of a nourishing diet could be your best defense. [1] Maternal undernutrition may be more prevalent in developed countries than the medical community recognizes. Insufficient intakes of vitamin A, vitamin D, vitamin K2, vitamin B6, biotin, choline, zinc, iron, iodine, glycine, and/or omega-3 fats are not uncommon. While outright birth defects may not result, a shortage of one or more of these nutrients could adversely impact a child, potentially contributing to physical or mental health challenges at birth and over his or her lifetime. This is still a controversial theory, but as the research expands on the “Developmental Origins of Disease” in the field of epigenetics (how the environment impacts our genes), I believe we will continue to see relationships between undernutrition and disease revealed. From Masterjohn C: Vitamins for Fetal Development [2] For the typical 5 foot 5 inch, 150 pound female, 20% of calories equates to 100 grams of protein when consuming 2000 calories in the first trimester, and 120 grams of protein when consuming 2400 calories in the third trimester. [i] Melendez-Hevia E, et al. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J Biosci. 2009; 34:853-872. [ii] Melendez-Hevia et al. A weak link in metabolism:….. [iii] Brawley L et al. Glycine rectifies vascular dysfunction induced by dietary protein imbalance during pregnancy. J Physiol. 2003;554:497-504. [iv] Melendez-Hevia E, De Paz-Lugo P, Cornish-Bowden A, Cardenas ML. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J Biosci. 200934(6):853-872. [v] Liberato SC et al. Effects of protein energy supplementation during pregnancy on fetal growth: a review of the literature focusing on contextual factors. Food Nutr Res. 2013;57(1). [vi] Rees WD, Wilson FA, Maloney CA. Sulfur amino acid metabolism in pregnancy: the impact of methionine in the maternal diet. J Nutr. 2006;136(6 Suppl):1701S-1705S. [vii] Lewis RM et al. Low serine hydroxymethlytransferase activity in the human placenta has important implications for glycine supply. J Clin Endocrinol Metab. 2005;90:1594-1598. [viii] Woessner JF, Brewer TH. Formation and breakdown of collagen and elastin in the human uterus during pregnancy and post-partum involution. Biochem J. 1963;89:75-89.

"Among 213 grandmother-mother-granddaughter triads, grandmothers in the top quarter of EtFOSAA exposure and with lower cholesterol levels had granddaughters with a 2.3-fold (95% CI 1.1-4.8) increased risk of abdominal and whole body overweight obesity compared to grandmothers in the bottom 25% of exposure." according to Barbara Cohn, PhD, of the Public Health Institute in Berkeley, California. https://www.medpagetoday.com/meetingcoverage/endo/85719
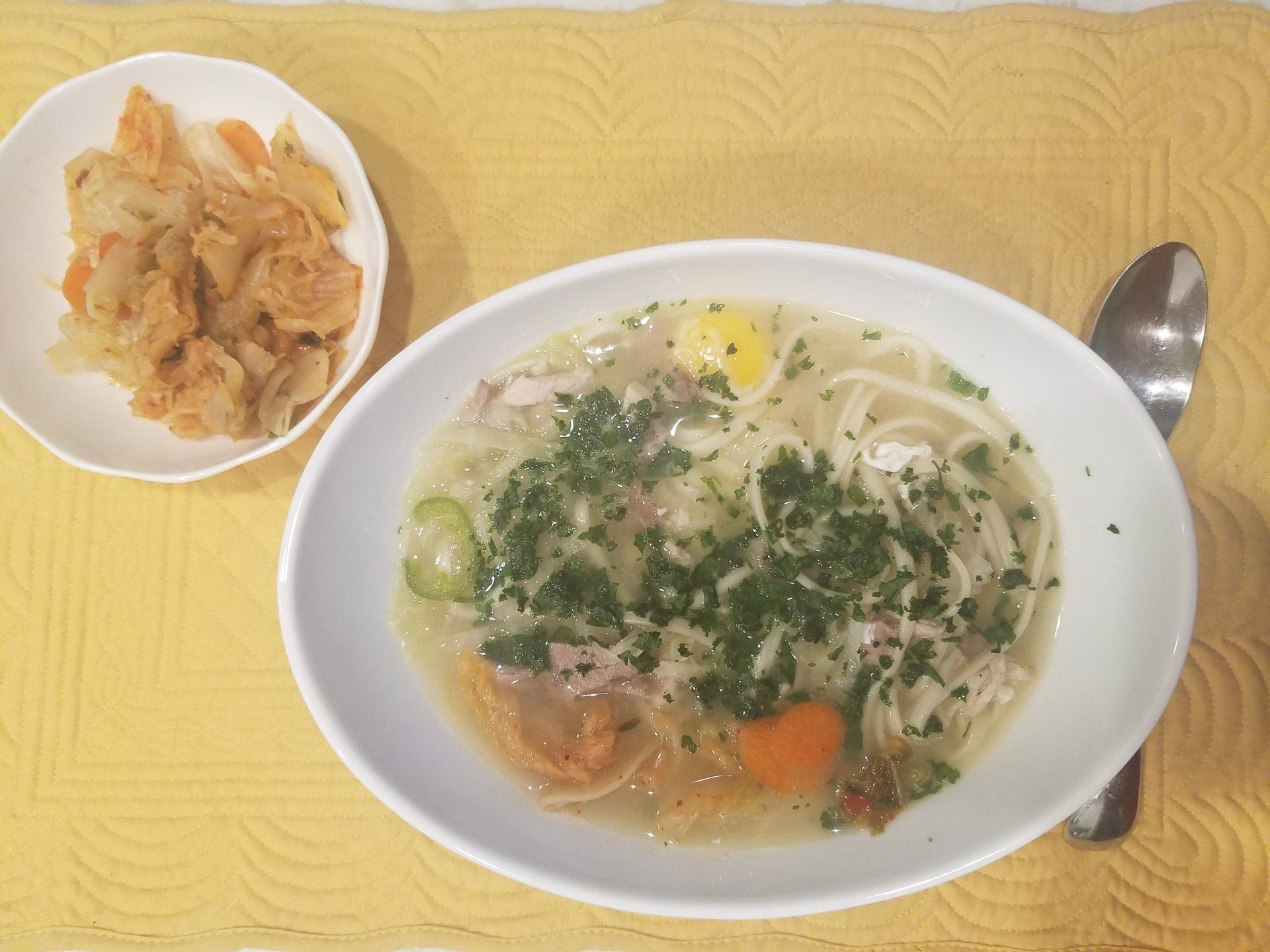
Home prepared soup is my favorite lunch (and sometimes breakfast!). I have been making this recipe for my husband and me at least four times each week. It takes a few minutes and covers so many nutrtional bases to support immune and overall health that I wanted to share it with you. 2 Servings Broth: put into medium size saucepan and simmer for 5-10 minutes. 24 ounces of bone broth, chicken or beef * 8-10 thin slices of ginger root 8-10 thin slices of jalapeno pepper 1-2 cloves of garlic, finely chopped 5 generous dashes of Tamari or other soy sauce 5 dashes of fish sauce 1/8 tsp fresh ground pepper salt to taste While broth is simmering, cook 2-4 ounces of soba noodles or fresh angel hair pasta per label directions (rice or buckwheat noodles are an option). Vegetables: choose two or more to add to soup, simmer an additional 4 minutes 1/3 cup of snow or snap peas, broken into thirds 2 leaves of kale, very finely sliced 1/4 cup finely chopped sauteed mushrooms 1/4 cup sliced water chestnuts, or 10 pieces of baby corn Protein: (choose one or more), add and simmer another minute. 1/2 cup finely cubed roast pork or chicken * 1/4 cup cubed firm tofu 1-2 whole eggs (cover to finish cooking these) 1/3 cup of cooked shrimp, cut into smaller pieces Fun to stir in to the pot just before serving: 2/3 cup fresh bean sprouts Add to taste at the table to each serving: 1/2 whole scallion, sliced Spoonful of chopped cilantro 1/4 cup of of kimchi 1 Tbsp lime juice * I purchase Butcher's Bone Broth at Publix https://butchersbyroliroti.com/ , or I make my own from roasted chicken or turkey wings, removing the meat after about one hour and simmering the bones and skins for 8-12 hours. Strain with fine mesh strainer and refrigerate extras.

I have been getting calls from women who don't think this is a good time to be planning for conception and want to postpone their visits. If you are personally trying to conceive the COVID-19 pandemic is likely adding to an already uncertain and stressful situation. Please read on, but also be aware that the Blue Cross Blue Shield of North Carolina plans that I accept are covering telehealth for nutritional counseling. Is It advisable to get pregnant now? The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine state:"At this time, very little is known about COVID-19, particularly related to its effect on pregnant women and infants, and there currently are no recommendations specific to pregnant women regarding the evaluation or management of COVID-19. Currently available data on COVID-19 does not indicate that pregnant women are at increased risk. However, pregnant women are known to be at greater risk of severe morbidity and mortality from other respiratory infections such as influenza and SARS-CoV. As such, pregnant women should be considered an at-risk population for COVID-19. Adverse infant outcomes (eg, preterm birth) have been reported among infants born to mothers positive for COVID-19 during pregnancy. However, this information is based on limited data and it is not clear that these outcomes were related to maternal infection. Currently it is unclear if COVID-19 can cross through the transplacental route to the fetus. In limited recent case series of infants born to mothers infected with COVID-19 published in the peer-reviewed literature, none of the infants have tested positive for COVID-19." https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019If If your medical doctor and/or OBGYN advises against trying to conceive at present, that of course is your best course of action. Yet, this might just be the very best time to really make your nutritional health your first priority. It has been documented that In traditional societies, women (and men) were given special nourishing foods at least 6 months before they were to get pregnant. https://www.westonaprice.org/health-topics/childrens-health/sacred-foods-for-exceptionally-healthy-babies-and-parents-too/ In fact, this is still a practice today in many areas of the world including Asia and South America. What actions can you take? This time of uncertainty could be an ideal opportunity to get your body ready for not only having a baby, but ready to handle any potential negative effects of COVID-19. This is a priority I am addressing with all of my patients - especially since some of the nutritional and holistic messages you may be hearing are not necessarily accurate. Supplements, along with a strong dietary foundation, can be helpful in supporting the immune system when well chosen and in the right doses. The best news is that the evidence we have so far is that pregnant women are still no more likely to contract the infection than the general population and that young children are at low risk for getting very sick. I hope and pray that we all weather this storm successfully and that you and your family stay well.

Whole milk and eggs do not threaten health, say studies ( from: http://www.nutritionatc.hawaii.edu/HO/2013/511.htm ) Milk and milk products like yogurt and cheese are commonly recommended as part of a healthy diet. These foods provide good sources of protein, calcium and several other essential nutrients. Because some dairy foods are high in fat and saturated fat, the lower-fat options typically are promoted as the most healthful options. Like higher-fat milk products, eggs are commonly maligned as a food bad for heart health due to their cholesterol content. However, two new extensive reviews of the scientific research on milk and eggs question both of these common recommendations. QUESTION: Do full-fat dairy foods adversely affect health when compared with low-fat and fat-free dairy foods? ANSWER: A thorough evaluation of the scientific research on high-fat dairy products was published in the January issue of the British Journal of Nutrition. Researchers from both the U.S. and Switzerland evaluated relationships between dairy fat consumption and the risks of obesity, type 2 diabetes and cardiovascular disease. They found that most studies do not support the low-fat recommendations. Q: Do high-fat dairy foods and eggs lead to obesity, diabetes and heart disease? A: Studies that followed people over time did not find a consistent link between obesity and the consumption of high-fat dairy foods. Somewhat surprisingly, several long-term studies indicated that people consuming the most high-fat dairy foods gained less weight than those who consumed less high-fat dairy products. Although it seems logical that lower-fat dairy products would be better for health (fewer calories and less fat and saturated fat), there are good reasons to question this assumption. During the past 40 years, while people in the U.S. largely switched from full-fat whole milk, yogurt and cheese to low-fat or skim options, the population steadily grew fatter. Would we be even fatter if we hadn't made the switch? Several studies indicate we might actually be leaner. Since the risks for diabetes and cardiovascular disease increase with body weight, it is not surprising the researchers found a lack of support for a link between high-fat dairy foods and the risk of developing diabetes or heart disease. Overall, there was more evidence that these foods may even be protective. Also in January, BMJ (previously British Medical Journal) published a major review of research studies on egg consumption and the risk of coronary heart disease and stroke. The authors reported that the results of their "meta-analysis" review "do not support that higher egg consumption is associated with elevated risk of coronary heart disease and stroke." Interestingly, the researchers found that higher egg consumption was associated with a reduced incidence of hemorrhagic stroke -- the type caused by bleeding into the brain. Q: Are the recommendations for choosing low-fat dairy products and avoiding eggs wrong? A: These new reviews certainly argue that the recommendations need to be reconsidered. It can be difficult to translate a review of studies conducted in various parts of the world into recommendations for a single country. The results of these studies do suggest that we do not need to fear these foods. Milk and eggs provide many nutrients and other components that can be important in an overall adequate diet. However, like any other type of foods, variety and moderation always make sense.



