Blogs
Recent Posts

There is probably nothing that tastes better than a fresh hot French Fry, dusted with salt and dipped in ketchup - YUM! One of my favorites! On the other hand, when I advise clients on "foods" to avoid or totally remove from their usual diet, the number one food on this (relatively short) list to avoid is fried foods. A no-brainer you are thinking - they are high in calories. Okay, yes, high in calories, but is that all that they are high in? Hardly. They also contain several toxic by-products from the repeated high heating of liquid frying oils. By toxic, I mean quite literally toxic to the human body. In fact, if someone has or had cancer, or has a high risk for cancer, I advise them to absolutely restrict their intake of all fried foods, along with other environmental toxins. Take a look at these conclusions made by scientists regarding the consumption of the frying oil present in all fried foods: Investigations have repeatedly demonstrated the heat-promoted generation of very high levels of highly toxic aldehydes in such products (particularly those fried in oils rich in in PUFAs - such as soybean and canola oil). , These findings have been available to the scientific, food and public health research communities since 1994. Used frying oils collected from domestic kitchens, fast-food retail outlets and restaurants, have confirmed the generation of these aldehydes at high concentrations during ‘on-site’ frying practices. Of critical importance to their public health risks as food-borne toxins , typical aldehydes produced during standard frying practices are absorbed from the gut into the circulation where they cause damage to cells, tissues, and essential organs. These toxic aldehydes (and other by-products) cause cellular stresses, and lead to adverse health effects on critical metabolic pathways - notably including on energy metabolism. Even with minimal or no heating, most of the oils used do not contain enough vitamin E to protect the highly oxidizable polyunsaturated fatty acids (PUFAs) they are high in. A Duke study of 4,000 children showed that potato chips, fried chicken and fish, and French fries were the top obesity-promoting foods. These foods also exert mutagenic (gene altering) and carcinogenic properties, teratogenic actions (which cause birth defects) and other striking pro-inflammatory effects. Finally, if you are trying to get pregnant, neither you or your partner should be eating fried foods more than once a week as adverse effects on sperm quality are well documented. We continue to learn more about the effects on female fertility, but there is a connection to oxidative stress, which is increased by consuming fried foods. These damaged oils stay in our bodies for up to 7 years!!!! With so many delicious foods available to eat in and out of the house, why endanger your health or fertility by eating fried foods? I can help guide you to better choices, please call me! Because of this knowledge, I rarely eat fried foods, with the exception of a couple of handfuls of tortilla chips when I eat at Mexican restaurants, a half-dozen French fries with my burger meal, or the occasional fried oyster, calamari, or shrimp appetizer for my birthday or my husband's birthday or other special occasion! Great short video on these dangers: https://www.theepochtimes.com/epochtv/are-vegetable-oils-killing-us-we-swapped-them-in-for-animal-fats-50-years-ago-5391966?utm_source=Morningbrief&src_src=Morningbrief&utm_campaign=mb-2023-07-13&src_cmp=mb-2023-07-13&utm_medium=email For more insights to this widespread dietary problem, here are two great blogs: https://www.alexfergus.com/blog/pufa-s-the-worst-thing-for-your-health-that-you-eat-everyday https://rustonsboneyard.com/whats-the-problem-with-vegetable-oil/ Dr. Perlmutter explains the mechanism of action behind the inflammatory effects of industrial seed oils: https://youtube.com/clip/UgkxePnsNRCUpqfH5MrWRNiHiiqwpQZdEY_o?si=JjXAp8xjlHg7x-Q8 And the oils don't have to be heated to cause problems like obesity and diabetes: https://info.bioticsresearch.com/researchforum/seed-oils-impact-on-health?utm_campaign=Research%20Forum&utm_medium=email&_hsenc=p2ANqtz-8WGyhIZHVtcMJdJq8q5VafEaUCQTtatMfoDI_CDP67CdsS5V9dEbOyWyS3iO4T6ojz_dUoSEYvA3qi23LlVMXzEDtgZRNP1_MdSFIs9Dc5sRqDmTM&_hsmi=371799084&utm_content=371799084&utm_source=hs_email&hsCtaTracking=f21aef02-d5b3-4511-8bf0-b603235f7eba%7C4945e873-a0e2-4fd9-9813-e7640cc56d84 Don't go to Chick-Fil-A more than once a week (if that): https://www.upi.com/Health_News/2019/01/24/Frequent-fried-food-increases-risk-for-obesity-heart-disease-death/4231548336486/ Your genes may be involved as well: https://www.sciencedaily.com/releases/2014/03/140318190027.htm "Oxidative stress (OS) has been identified to play a key role in the pathogenesis of subfertility in both males and females. The adverse effects of OS on sperm quality and functions have been well documented. In females, on the other hand, the impact of OS on oocytes and reproductive functions remains unclear. This imbalance between pro-oxidants and antioxidants can lead to a number of reproductive diseases such as endometriosis, polycystic ovary syndrome (PCOS), and unexplained infertility. Pregnancy complications such as spontaneous abortion, recurrent pregnancy loss, and preeclampsia, can also develop in response to OS. Studies have shown that extremes of body weight and lifestyle factors such as cigarette smoking, alcohol use, and recreational drug use can promote excess free radical production, which could affect fertility. Exposures to environmental pollutants are of increasing concern, as they too have been found to trigger oxidative states, possibly contributing to female infertility." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527168/ There are ways to make fried foods more safe and less prone to causing oxidative stress in the body, but you cannot really be sure if the restaurant etc. where you purchase food is utilizing the best practices: https://www.researchgate.net/publication/268408525_Nonnutrient_Antioxidants_and_Stability_of_Frying_Oils Toxic aldehyde generation in and food uptake from culinary oils during frying practices: nature.com/articles/s41598-019-39767-1 The USDA recommends that people consume more liquid vegetable oils to get sufficient vitamin E, but this is clearly not the way to do it. Better to eat fresh nuts and seeds, whole grains, dark leafy greens, pastured eggs, and avocados, and supplement as needed with a mixed vitamin E, such as Jarrow Famil-E: https://academic.oup.com/jn/article-abstract/81/4/335/4779307?redirectedFrom=fulltext

Collagen protein from the very start. While clearly beneficial in our senior years, there is a very different stage of life when collagen protein intake is equally if not even more important. That time is during fetal development. [i] Even if you are well past your child-bearing years, please read on as you may be able to share this helpful information with expectant parents. Many women who I help come in with hormonal problems, infertility, or pregnancy complicated by obesity or poor blood sugar control. The women I don’t see anywhere near as often are those that do not experience problems conceiving or carrying a baby to term. This is a real shame because all women can benefit from a thorough review of their diet by a knowledgeable dietitian or nutritionist, before, during, and after pregnancy. Whether pregnant or trying to conceive, my patients consistently tell me how valuable the information I shared with them was and how glad they were to have met with me. In the words of one mother-to-be, “I didn’t know what I didn’t know.” Unfortunately, many women continue to have gaps in their prenatal nutrition despite following the recommended dietary guidelines and receiving the best obstetrical care. Could these gaps lead to problems for a woman or her baby? Based on the growing body of research in reproductive nutrition, the potential is there. [1] My goal is to see all women be fully nourished during the critical life stages of pregnancy and lactation. In my practice, one of the most frequent recommendations I make to pregnant patients is that they consume more collagen protein. They are surprised to learn that daily servings of skin-on organic chicken, gelatin dishes, and soups made with bone broth are important parts of their prenatal diet. And I have yet to meet with an expectant mother that was already in the habit of eating these nourishing foods prior to our first appointment. One of the main reasons collagen protein appears to be essential during pregnancy is, once again, that little amino acid glycine. According to nutritional scientists, “the shortage of glycine may become serious in conditions such as pregnancy.” [ii] What might “serious” mean for a pregnant woman and her baby? Pregnancy creates a higher demand for glycine due to the increased collagen and elastin synthesis taking place in the expanding uterus and stretching skin. As a result, glycine may become a limiting factor for protein synthesis in the developing fetus. Without enough available glycine, there is the possibility that fetal growth will be restricted, albeit to an unknown extent. Additionally, in studies on pregnant rats, glycine supplementation reversed the high blood pressure and the blood vessel dysfunction that occurred when they were fed lower protein diets. [iii] These findings point to an important (pivotal per authors) role for dietary glycine in the adaptations required during pregnancy to support healthy maternal circulation. Recall from chapter 3 that some scientists consider glycine to be one of the conditionally-essential amino acids because the human body cannot synthesize enough glycine to meet more than its most basic survival needs. There are numerous health benefits to consuming sufficient quantities of glycine through diet, 10 grams per day appears to be about optimal. [iv] And while 10 grams may be sufficient for almost every healthy adult, it is almost certain that a moderately higher amount would be beneficial during pregnancy, especially during the last two trimesters when the most rapid growth occurs. To better understand the role of glycine, we need to look at it in the context of the overall diet. It is generally recommended that a woman consume an additional 25 grams of protein per day during the second and third trimesters of pregnancy, or a total of 71 grams protein per day. A lot more protein is not advisable. High protein diets that exceed 20% of calories from protein can impair fetal growth, according to a 2013 review of the research. [v] [2] And an excess of the amino acid methionine relative to glycine is not optimal either. Too much methionine not only increases the need for glycine but may lead to other undesirable effects on the child’s long-term physiology. [vi] Where would an excess of methionine come from? From high protein diets that are often thought of as healthy, and especially ones with predominantly lean muscle protein, like chicken breast and lean meat. So whether it is the total amount of protein or methionine, or the ratio of methionine to glycine consumed, it is important to make sure that the sources of protein are balanced, avoiding too little as well as too much. Nutritionists often referred to this as the “Goldilocks Principle” and it can be applied to almost any nutrient, supplement, or food that we consume. Of course collagen protein, although an excellent source of glycine and other amino acids, is just one component of a nourishing diet! When I am asked what the perfect meal for a pregnant woman is, I answer: a great homemade soup made with collagen-rich bone broth, one to two ounces of meat, poultry, organ meat, or safe seafood, one ounce of soft-cooked tendons such as in the traditional Vietnamese dish Pho, plenty of fresh leafy greens, a small potato or sweet potato, a half-cup of a favorite type of legume, a whole egg or even better two egg yolks, a bit of seaweed rich in iodine, and a handful of cilantro or other green herbs. On the side would be a fermented vegetable like sauerkraut. This would be accompanied by a good source of calcium such as a grass-fed cheese or yogurt, along with a fresh fruit for dessert, topped off by a little sunshine for vitamin D! Come to think of it, this is a perfect meal for just about anybody, at any time! Recovery after delivery. Collagen protein consumed throughout pregnancy could have further benefits after delivery. We already know that pregnant women need more collagen protein because a high proportion of them have been shown to have a glycine insufficiency. [vii] It has also been shown that with each pregnancy, the collagen and elastin content of a women’s uterus increases. [viii] Stretch marks happen when a women’s belly expands faster than her skin can keep up with, causing the collagen and elastin fibers in your skin to break. Because collagen protein has been shown to increase the elasticity of the skin, it just might minimize the appearance of those annoying stretch marks. Other than not gaining excessive weight during pregnancy, medical experts don’t know how to prevent stretch marks. Collagen protein in the context of a nourishing diet could be your best defense. [1] Maternal undernutrition may be more prevalent in developed countries than the medical community recognizes. Insufficient intakes of vitamin A, vitamin D, vitamin K2, vitamin B6, biotin, choline, zinc, iron, iodine, glycine, and/or omega-3 fats are not uncommon. While outright birth defects may not result, a shortage of one or more of these nutrients could adversely impact a child, potentially contributing to physical or mental health challenges at birth and over his or her lifetime. This is still a controversial theory, but as the research expands on the “Developmental Origins of Disease” in the field of epigenetics (how the environment impacts our genes), I believe we will continue to see relationships between undernutrition and disease revealed. From Masterjohn C: Vitamins for Fetal Development [2] For the typical 5 foot 5 inch, 150 pound female, 20% of calories equates to 100 grams of protein when consuming 2000 calories in the first trimester, and 120 grams of protein when consuming 2400 calories in the third trimester. [i] Melendez-Hevia E, et al. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J Biosci. 2009; 34:853-872. [ii] Melendez-Hevia et al. A weak link in metabolism:….. [iii] Brawley L et al. Glycine rectifies vascular dysfunction induced by dietary protein imbalance during pregnancy. J Physiol. 2003;554:497-504. [iv] Melendez-Hevia E, De Paz-Lugo P, Cornish-Bowden A, Cardenas ML. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J Biosci. 200934(6):853-872. [v] Liberato SC et al. Effects of protein energy supplementation during pregnancy on fetal growth: a review of the literature focusing on contextual factors. Food Nutr Res. 2013;57(1). [vi] Rees WD, Wilson FA, Maloney CA. Sulfur amino acid metabolism in pregnancy: the impact of methionine in the maternal diet. J Nutr. 2006;136(6 Suppl):1701S-1705S. [vii] Lewis RM et al. Low serine hydroxymethlytransferase activity in the human placenta has important implications for glycine supply. J Clin Endocrinol Metab. 2005;90:1594-1598. [viii] Woessner JF, Brewer TH. Formation and breakdown of collagen and elastin in the human uterus during pregnancy and post-partum involution. Biochem J. 1963;89:75-89.

"Among 213 grandmother-mother-granddaughter triads, grandmothers in the top quarter of EtFOSAA exposure and with lower cholesterol levels had granddaughters with a 2.3-fold (95% CI 1.1-4.8) increased risk of abdominal and whole body overweight obesity compared to grandmothers in the bottom 25% of exposure." according to Barbara Cohn, PhD, of the Public Health Institute in Berkeley, California. https://www.medpagetoday.com/meetingcoverage/endo/85719
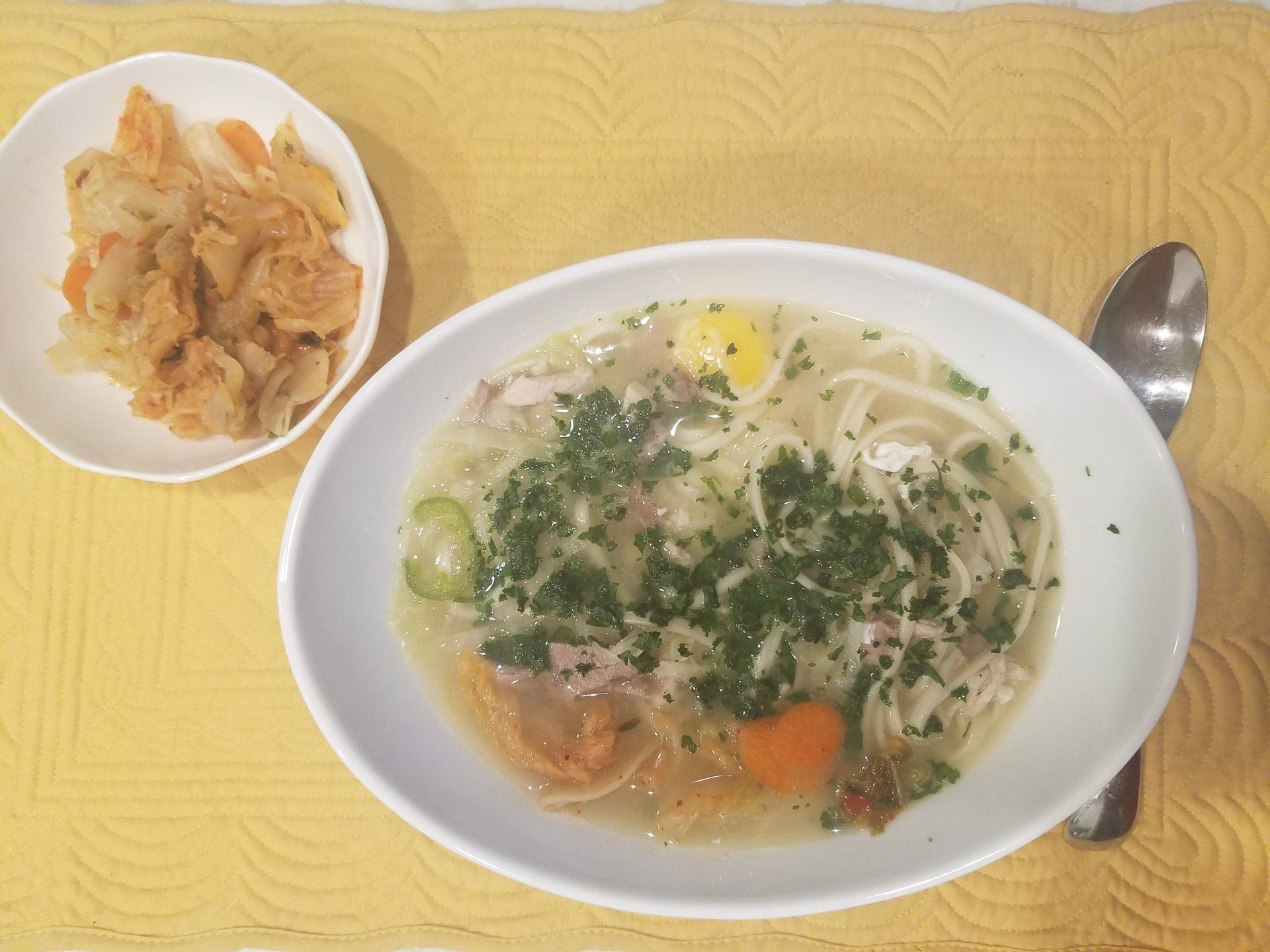
Home prepared soup is my favorite lunch (and sometimes breakfast!). I have been making this recipe for my husband and me at least four times each week. It takes a few minutes and covers so many nutrtional bases to support immune and overall health that I wanted to share it with you. 2 Servings Broth: put into medium size saucepan and simmer for 5-10 minutes. 24 ounces of bone broth, chicken or beef * 8-10 thin slices of ginger root 8-10 thin slices of jalapeno pepper 1-2 cloves of garlic, finely chopped 5 generous dashes of Tamari or other soy sauce 5 dashes of fish sauce 1/8 tsp fresh ground pepper salt to taste While broth is simmering, cook 2-4 ounces of soba noodles or fresh angel hair pasta per label directions (rice or buckwheat noodles are an option). Vegetables: choose two or more to add to soup, simmer an additional 4 minutes 1/3 cup of snow or snap peas, broken into thirds 2 leaves of kale, very finely sliced 1/4 cup finely chopped sauteed mushrooms 1/4 cup sliced water chestnuts, or 10 pieces of baby corn Protein: (choose one or more), add and simmer another minute. 1/2 cup finely cubed roast pork or chicken * 1/4 cup cubed firm tofu 1-2 whole eggs (cover to finish cooking these) 1/3 cup of cooked shrimp, cut into smaller pieces Fun to stir in to the pot just before serving: 2/3 cup fresh bean sprouts Add to taste at the table to each serving: 1/2 whole scallion, sliced Spoonful of chopped cilantro 1/4 cup of of kimchi 1 Tbsp lime juice * I purchase Butcher's Bone Broth at Publix https://butchersbyroliroti.com/ , or I make my own from roasted chicken or turkey wings, removing the meat after about one hour and simmering the bones and skins for 8-12 hours. Strain with fine mesh strainer and refrigerate extras.

I have been getting calls from women who don't think this is a good time to be planning for conception and want to postpone their visits. If you are personally trying to conceive the COVID-19 pandemic is likely adding to an already uncertain and stressful situation. Please read on, but also be aware that the Blue Cross Blue Shield of North Carolina plans that I accept are covering telehealth for nutritional counseling. Is It advisable to get pregnant now? The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine state:"At this time, very little is known about COVID-19, particularly related to its effect on pregnant women and infants, and there currently are no recommendations specific to pregnant women regarding the evaluation or management of COVID-19. Currently available data on COVID-19 does not indicate that pregnant women are at increased risk. However, pregnant women are known to be at greater risk of severe morbidity and mortality from other respiratory infections such as influenza and SARS-CoV. As such, pregnant women should be considered an at-risk population for COVID-19. Adverse infant outcomes (eg, preterm birth) have been reported among infants born to mothers positive for COVID-19 during pregnancy. However, this information is based on limited data and it is not clear that these outcomes were related to maternal infection. Currently it is unclear if COVID-19 can cross through the transplacental route to the fetus. In limited recent case series of infants born to mothers infected with COVID-19 published in the peer-reviewed literature, none of the infants have tested positive for COVID-19." https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019If If your medical doctor and/or OBGYN advises against trying to conceive at present, that of course is your best course of action. Yet, this might just be the very best time to really make your nutritional health your first priority. It has been documented that In traditional societies, women (and men) were given special nourishing foods at least 6 months before they were to get pregnant. https://www.westonaprice.org/health-topics/childrens-health/sacred-foods-for-exceptionally-healthy-babies-and-parents-too/ In fact, this is still a practice today in many areas of the world including Asia and South America. What actions can you take? This time of uncertainty could be an ideal opportunity to get your body ready for not only having a baby, but ready to handle any potential negative effects of COVID-19. This is a priority I am addressing with all of my patients - especially since some of the nutritional and holistic messages you may be hearing are not necessarily accurate. Supplements, along with a strong dietary foundation, can be helpful in supporting the immune system when well chosen and in the right doses. The best news is that the evidence we have so far is that pregnant women are still no more likely to contract the infection than the general population and that young children are at low risk for getting very sick. I hope and pray that we all weather this storm successfully and that you and your family stay well.

Whole milk and eggs do not threaten health, say studies ( from: http://www.nutritionatc.hawaii.edu/HO/2013/511.htm ) Milk and milk products like yogurt and cheese are commonly recommended as part of a healthy diet. These foods provide good sources of protein, calcium and several other essential nutrients. Because some dairy foods are high in fat and saturated fat, the lower-fat options typically are promoted as the most healthful options. Like higher-fat milk products, eggs are commonly maligned as a food bad for heart health due to their cholesterol content. However, two new extensive reviews of the scientific research on milk and eggs question both of these common recommendations. QUESTION: Do full-fat dairy foods adversely affect health when compared with low-fat and fat-free dairy foods? ANSWER: A thorough evaluation of the scientific research on high-fat dairy products was published in the January issue of the British Journal of Nutrition. Researchers from both the U.S. and Switzerland evaluated relationships between dairy fat consumption and the risks of obesity, type 2 diabetes and cardiovascular disease. They found that most studies do not support the low-fat recommendations. Q: Do high-fat dairy foods and eggs lead to obesity, diabetes and heart disease? A: Studies that followed people over time did not find a consistent link between obesity and the consumption of high-fat dairy foods. Somewhat surprisingly, several long-term studies indicated that people consuming the most high-fat dairy foods gained less weight than those who consumed less high-fat dairy products. Although it seems logical that lower-fat dairy products would be better for health (fewer calories and less fat and saturated fat), there are good reasons to question this assumption. During the past 40 years, while people in the U.S. largely switched from full-fat whole milk, yogurt and cheese to low-fat or skim options, the population steadily grew fatter. Would we be even fatter if we hadn't made the switch? Several studies indicate we might actually be leaner. Since the risks for diabetes and cardiovascular disease increase with body weight, it is not surprising the researchers found a lack of support for a link between high-fat dairy foods and the risk of developing diabetes or heart disease. Overall, there was more evidence that these foods may even be protective. Also in January, BMJ (previously British Medical Journal) published a major review of research studies on egg consumption and the risk of coronary heart disease and stroke. The authors reported that the results of their "meta-analysis" review "do not support that higher egg consumption is associated with elevated risk of coronary heart disease and stroke." Interestingly, the researchers found that higher egg consumption was associated with a reduced incidence of hemorrhagic stroke -- the type caused by bleeding into the brain. Q: Are the recommendations for choosing low-fat dairy products and avoiding eggs wrong? A: These new reviews certainly argue that the recommendations need to be reconsidered. It can be difficult to translate a review of studies conducted in various parts of the world into recommendations for a single country. The results of these studies do suggest that we do not need to fear these foods. Milk and eggs provide many nutrients and other components that can be important in an overall adequate diet. However, like any other type of foods, variety and moderation always make sense.

by Chris Kresser, M.S. (this is a repost of extremely important summary of recent findings) In one of the first article series I (Chris Kresser) ever wrote, 9 Steps To Perfect Health, I referred to the “Three Horsemen of the Diet Apocalypse.” These are the three food categories in the standard American diet (which is now prevalent in all industrialized countries) that I believe have had the most harmful impact on our health. They are: Sugar Flour Industrial seed oils Removing these three foods should always be the starting place for someone who wants to improve their diet, but may not be ready for a full Paleo Reset or another stricter approach. Most people have a good understanding of why flour and sugar are harmful, from their impact on blood sugar to how they affect the gut microbiome. But what about industrial seed oils? Well, a new study published in the journal Endocrinology makes this clear. The authors found that soybean oil, which is the most widely consumed edible oil in the United States (comprising about 7 percent of the calories the average American eats!), not only contributes to obesity and diabetes, but may also increase the risk of neurological conditions like autism, Alzheimer’s disease, anxiety, and depression. How does this happen? The researchers discovered that soybean oil has pronounced effects on the hypothalamus, a small region of the brain that regulates weight, body temperature, and metabolism (among other things). They also found that soybean oil consumption changed the expression of over 100 genes involved in everything from energy metabolism to proper brain function. Interestingly, coconut oil produced very few changes in the hypothalamic genes that soybean oil altered. This finding contradicts conventional wisdom that polyunsaturated fats (like soybean oil) are healthier than saturated fats (like coconut oil). Caveat: this research was performed in mice, so we can’t be certain that these findings would also apply to humans. That said, the mechanisms are likely similar, and in my mind, these data are certainly enough to warrant a large reduction in soybean oil consumption. Where is soybean oil found in the diet? Processed, refined, packaged, and—sadly, yes—restaurant foods. (Fortunately, some higher-quality restaurants are starting to avoid using it, and consumers have power here, so it doesn’t hurt to ask your favorite restaurants if they cook with it.) So, cooking most of your food at home and avoiding packaged foods—which is a good idea on many levels—is the best way to reduce your consumption of soybean oil. In health, Chris https://chriskresser.com/how-industrial-seed-oils-are-making-us-sick/

This week (1/7/2020), a study that measured changes in fertility rates when men were given a daily supplement containing zinc (30 mg) and folic acid (5,000 mcg) for 6 months made the medical news round-up. This was a fairly large study with about 1800 couples whose male partners completed the 6-month trial of supplementation. The researchers found the zinc and folic acid combination did not increase the birth rates over those whose male partner only took a placebo. And in fact, according the the researchers, "Men taking the supplement combination also saw no difference in sperm quality parameters such as sperm count, movement, or formation. In fact, this group showed lower sperm quality due to greater sperm DNA fragmentation, the researchers reported in JAMA. Men in the supplementation group had an average of 29.7% DNA fragmentation, versus 27.2% in the placebo group (mean difference 2.4%, 95% CI 0.5%-4.4%)." The headline from MedPage Today: "Men: Forget the Zinc and Folic Acid to Boost Fertility" Furthermore, "A fertility specialist not involved in the study commented, When a patient has good nutrition, Drews said that "the idea of enhancing male or female fertility through the use of nutritional or vitamin supplements makes little teleological evolutionary sense."" Unfortunately, this headline and expert comment are highly misleading. The key question here is "how do we measure and ensure good nutrition?" Do we just throw darts at a board, as this study does? Do we give excessively high doses of a synthetic form of folic acid, which when taken by a women during pregnancy is linked to a higher risk of autism spectrum disorder in their children? This study makes so little sense and is on the verge of being unethical in its approach. I doubt they would every give women who is trying to conceive this type of one-size-fits all supplementation, but somehow it is okay for men because sperm is only half the equation? (sarcasm here). My advice: for couples who are considering improving the father's nutrition before conceiving, please do this with a professional's guidance who will consider your personalized needs. Every good functional health care practitioner would support this strategy. Here is the comment I posted on the MedPage today site: 'What evidence is there to support men needing 5 mg/day of folic acid, especially considering that most people consume more than adequate amounts from the enriched grain products they eat? Consider that this high dose will lead to measurable levels of unmetabolized folic acid in the body, with unknown and possibly negative consequences. This is another study that confuses the issue as it is a one-size-fits-all supplementation scheme. Many men may benefit from zinc supplementation if consuming a low intake of red meat and/or plant-based diet, and doses should ideally be tailored to their needs and supported by checking plasma zinc levels. Also, copper often needs to be supplemented along with zinc supplement in a 1:15 ratio. It is disappointing to see money wasted on research that as usual does not tailor repletion of nutrients to patients'actual needs. This is what experienced registered dietitians do every day with their patients, address shortfalls and excesses in the diet according to individual needs." Looking forward to seeing if anyone else expresses these same reservations about the study. https://www.medpagetoday.com/endocrinology/infertility/84250?xid=nl_mpt_DHE_2020-01-08&eun=g270711d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=Daily%20Headlines%20Top%20Cat%20HeC%20%202020-01-08&utm_term=NL_Daily_DHE_dual-gmail-definition

Sweat Loss Measurement: Studies conducted during exercise show that people vary significantly in the amount of sweat they lose and in the amount of sodium lost in sweat. Since these measurements are difficult to make, new research is developing skin sensor technology that promises to make it easy to measure the amount of sweat lost and the amount of salts in that sweat.

A majority of women I see choose to limit the amount of red meat they eat. While for some this may be a good idea, many do not realize that red meat, especially beef, is their best dietary source of the essential minerals zinc and iron. Younger women with regular menstrual cycles are at a much higher risk for iron deficiency, and those who take oral contraceptives are at a higher risk for zinc deficiency. I'll discuss how to address iron deficiency and why it is important in the future. Today I want to share a study that demonstrates that higher intakes of zinc (from a supplement) supports more rapid weight loss and improves other markers of health in adults with obesity. In a recent randomized study, two groups of 20 adults each were assigned to take a zinc supplement (30 mg) or a placebo daily. Both groups reduced their calorie intake to 300 calories less than their estimated needs. After 4 months, both groups lost weight, however, the individuals taking zinc lost an average of 10 lbs as compared to the placebo group who averaged only a 3.3 lb weight loss. The supplemental zinc also lowered inflammation, insulin resistance, and even appetite scores. The authors stated that zinc deficiency is suprisingly prevalent in individuals with obesity, and this was observed in these 40 individuals whose average serum zinc level was 65 mcg/dL at the start of the study, rising signficantly after the 4 months. Note that ideal blood levels of zinc are between 80-120 mcg/dL. I often request that doctors check blood zinc levels for my patients, and when they do, I find that over half of my patients have lower than optimal zinc levels. Red meat provides 9 mg of zinc in a 3-ounce portion, while a single oyster supplies over 6 mg of zinc. A women's daily need for zinc is 8-12 grams, the higher amount is during breastfeeding. While food nutrient content databases indicate that certain plant foods like legumes and whole grains contain a fair amount of zinc, plant sources of zinc are bound to phytates which make it very difficult to absorb. If a women is a vegetarian or vegan, she is at higher risk for a low intake of zinc. Cheese and other dairy foods contain a moderate amount of zinc, so a vegan diet is typically the lowest in available zinc. Of note, this study is not really suprising to me because the patients who are most successful at their weight loss goals are the ones who actviely address their micronutrient deficiencies under my guidance. Overweight and obesity are multifactorial problems and it takes a practitioner with extensive experience to help uncover and address the causes. Zinc supplementation may enhance weight loss in obese adults on a restricted calorie diet . Researchers recruited 40 adults with obesity, and randomly assigned them to take either zinc (30 mg / day) or placebo. Both groups were placed on a restricted calorie diet (~300 kcal lower than their estimated energy requirement). After fifteen weeks, both groups experienced weight loss, but the zinc group showed an average weight loss of 4.6 kg (about ten pounds), compared to 1.5 kg in the placebo group (around 3.3 pounds). Compared to the placebo group, those taking zinc experienced improved body weight management, inflammatory biomarkers, appetite scores, and insulin resistance. Subclinical zinc deficiency is surprisingly prevalent in obese individuals, and this group was a pretty good example of this phenomenon - mean serum zinc levels in the experimental group were below the normal range at baseline (65.2 ± 5.9μg/dL), and rose significantly after the supplement regimen.

As the most abundant mineral in your body, calcium is extremely important for you overall health. This essential mineral makes up much of your bones and teeth and plays a role in heart health, muscle function, and nerve signaling. The recommended daily intake of calcium is 1,000 mg per day for most adults, although women over 50 and everyone over 70 should get 1,200 mg per day, pregnant and lactating women need 1000-1300 mg, and growing children aged 4–18 should also consume 1,300 mg. Popular calcium-rich foods include dairy products like milk, cheese, and yogurt. However, certain seafood, leafy greens, legumes, dried fruit, tofu and foods fortified with calcium are also very good sources. Below is a chart listing foods that are commonly known to be good or excellent sources of calcium. Scroll through to see if you are meeting your daily calcium needs. Other foods do provide calcium, but typically less than 50 mg per serving.

Collagen has a unique amino acid composition and a distinct role in human anatomy. For instance, collagen protein is a more concentrated source of glycine, proline, and the modified amino acid hydroxyproline, as compared to other dietary proteins, making it a potentially more effective choice when the clinical goal is related to collagen as a structural protein. According to a study published last Thursday in Nutrients, researchers demonstrated the efficacy of specific collagen supplementation in improving body composition in active men. This double-blinded, placebo-controlled, randomized clinical trial consisted of 57 active men over a twelve-week period. Each individual participated in weight training 3 times a week and supplemented with 15 grams of collagen peptides or a placebo. Assessments included strength testing, bioimpedance analysis (BIA) and muscle biopsies. Pre-training biopsies were taken, followed by a second one to analyze the acute effects of collagen peptide supplementation and training. Results showed a significant increase in fat free mass compared to the placebo. In addition, body fat mass was unchanged in the collagen supplementation group compared to a significant increase in the placebo group. One of the novelties of this study was the use of biopsies. Although the muscle fiber cross-sectional area was not significantly different between the groups, the increase in the fat free mass after the collagen supplementation was not only associated with hypertrophy of the contractile muscle cells but possibly an increase in connective tissue compared to the placebo group. Many people often think of whey protein or branched-chain amino acids (BCAAs) for improving body composition and preserving lean tissue mass, as leucine is the most potent amino acid to stimulate muscle protein synthesis. While this is true, collagen peptides have been receiving more and more attention in this area. However, it is difficult to consume adequate amounts of collagen through diet alone, as its richest sources—animal skins, bone broth, and tendons— are not typically part of the modern Western diet. The body is not only composed of complete proteins, but is 25% to 30% collagen. Collagen protein is renewed at comparable rates to other proteins in the body, such as in muscle. It is important to note that collagen also makes up a significant component of many tissues such as 65% to 80% in tendons, 70% in ligaments, and 50% in cartilage. This is significant because many musculoskeletal injuries are tendon tears, so it makes sense for anyone living an active lifestyle to obtain adequate collagen through supplementation. Other areas where collagen supplementation may be of benefit include skin health, sarcopenia, osteoporosis, blood pressure, and insulin resistance. It important to use a quality collagen supplement backed by research, and is a low molecular weight to optimize absorption and efficacy. By Michael Jurgelewicz, DC, DACBN, DCBCN, CNS Source: Kirmse M, Oertzen-Hagemann V, et al. Prolonged Collagen Peptide Supplementation and Resistance Exercise Training Affects Body Composition in Recreationally Active Men. Nutrients. 2019 May 23;11(5).
A study by scientists at Boston Children's Hospital and Brigham and Women's Hospital points to the high probability that the growing epidemic of pediatric food allergy is due to the absence of certain"good" or "probiotic" bacteria in a child's gut , "The loss of these bacteria acts as a switch that makes children susceptible to food allergy," says Talal Chatila, MD, director of the Food Allergy Program at Boston Children's and a senior author on the paper. While the study was conducted in mice, it suggests a viable way to protect children from developing food allergies -- and possibley even reverse food allergies in children who already have it. The number of Americans who suffer from food allergy has risen sharply over the last decade to as many 32 million, and almost one of every dozen children are affected. One suggestion is that certain lifestyle factors -- including an increase in C-sections, a decline in breastfeeding, and the increased use of antibiotics -- are disrupting the normal microbial balance in the gut, depriving infants of the "good" bacteria (and food for that good bacteria a.k.a. "prebiotics") that prepare their immune systems to recognize food as safe to consume. The team of scientists initially tested this hypothesis by studying gut bacteria in babies with and without food allergies. They collected stool samples from 56 food-allergic patients and 98 patients without food allergies. They then analyzed those samples for changes in bacterial content. This showed that the bacteria in the "poop" of babies with food allergies differed from those who were not allergice. But did those bacterial differences play a role in causing food allergies? To find out, the team then placed fecal bacteria from the babies into a special strain of allergy-prone mice. They fed the mice small doses of chicken egg protein to sensitize their immune systems to this allergen, then challenged the mice with a large dose. The results: Mice that had been given "poop" bacteria from food-allergic babies went into the life-threatening allergic reaction called anaphylaxis. The poop bacteria from food-allergic babies did not protect against food allergy, whereas the bacteria from non-allergic babies did. To find out which bacteria might be offering that protection, a mix of six bacterial species from the order Clostridiales were given to the mice; these animals were protected from food allergy to chicken egg protein, whereas mice given other common bacteria were not. "If you give them the right bacteria, the Clostridia, they're completely resistant to food allergy," Chatila says. A second mix of unrelated bacteria from the order Bacteroidales was also protective. And finally, when the team treated mice that already had food allergy with the Clostridiales or Bacteroidales mixes, they found those therapies completely suppressed the animals' allergic reactions. Chatila believes the study proves that the loss of protective gut bacteria is a critical factor in food allergy. "At the very least it is a fundamental mechanism. And more likely, in my mind, it is the fundamental mechanism on which other things can be layered," he says. Chatila and colleagues believe their findings will eventually lead to new treatments that prevent the development of food allergies in newborns at risk. The treatments might take the form of probiotics -- mixes of beneficial bacteria -- or drugs that prime the immune system in the same way. And for the millions who already suffer from food allergies, the same treatments may be able to reverse their disease. In adult mice that had become food-allergic, they could suppress their disease by introducing the good bacteria, which means there is the potential to treat somebody with established food allergy and reset their immune system in favor of tolerance. The promising results in mice will have to be duplicated in humans. But the exciting news is that a first-of-its-kind clinical trial is being conducted at Boston Children's to test the safety and efficacy of fecal transplants in adults with peanut allergy. And Chatila notes that several companies are already preparing bacterial mixes for clinical trials. "If the race continues with the same intensity, or accelerates, I think you'll see a product on the market within five years," he predicts.

This post is written by supplement company that produces high quality products: Designs for Health. I recommend and personally use a few of their supplements for PCOS: Sensitol and N-Acetyl Cysteine. I also love their Whole Body Collagen. I can guide you in appopriate use of supplements and offer my patients a significant discounts on professional grade products, including those from Designs for Health. My comments are in italics. Polycystic ovary syndrome (PCOS) is one of the most prevalent conditions affecting women’s reproductive health. As practitioners, we are well aware that the body’s hormone network is highly complex and interwoven with many other metabolic pathways, so PCOS is not just a hormonal condition, but an endocrine disorder, as well. Characterized by polycystic ovaries, chronic anovulation, and hyperandrogenism, the leading symptoms of PCOS include irregular menstrual cycles, hirsutism, acne and infertility. Insulin resistance, compensatory hyperinsulinemia, and reduced insulin clearance are primary metabolic abnormalities associated with the development of PCOS . Compared to age and BMI-matched controls with prediabetes (but no hyperandrogenism and ovulatory disorders), those with PCOS have significantly higher levels of insulin 2 hours following an oral glucose tolerance test and a lower metabolic clearance rate of insulin (MCRI), but a similar degree of insulin sensitivity . Therefore, insulin clearance may be a factor that distinguishes the endocrine dysfunction of PCOS from that of type 2 diabetes. Similarly, obesity is often a characteristic associated with PCOS and has led many to believe that type 2 diabetes was an underlying cause of PCOS; however, rising numbers of lean women are also presenting with PCOS and confusing the theory that insulin resistance in PCOS is a result of obesity. In a meta-analysis study comparing insulin resistance and sensitivity among obese or non-obese women with PCOS, and obese or non-obese healthy controls, it was found that obesity alone did not have a statistically significant effect on insulin resistance and sensitivity (although obesity certainly increased insulin resistance), but the presence of PCOS had a greater effect on insulin resistance than was caused by obesity alone. Another study seeking to understand how insulin resistance in PCOS is independent of obesity compared insulin resistance and β cell function in lean PCOS patients with obese PCOS controls. Interestingly, the lean PCOS patients had a similar β cell function and insulin resistance as compared to controls. Additionally, fasting c-peptide and its ratio to glucose were significantly higher in lean patients compared to controls. Together, these results indicate that the insulin metabolism of PCOS is, again, independent of obesity. Although insulin-sensitizing pharmaceuticals are traditional recommendations for addressing the hyperinsulinemia associated with PCOS, more conservative and natural approaches often focus on a low-sugar, Paleolithic or Ketogenic styles to control blood sugar and insulin levels. While these diets most certainly play a crucial role in optimizing the health of the whole body and balancing blood sugar levels, they are most effective in those who also experience obesity coupled with PCOS. As weight is better managed by rebalancing blood sugar, insulin is better regulated. However, in the lean population with PCOS (and even in many of the obese patients with severe cases of PCOS), a low-sugar diet alone is not enough to address the insulin complications. Inositol Various botanicals and nutraceuticals are helpful in improving insulin resistance and sensitivity when the diet is not enough. In a randomized controlled trial , 50 women with PCOS, insulin resistance, and hyperinsulinemia were given either 4 g per day of myo-inositol or 1500 mg per day of metformin, the commonly prescribed insulin-sensitizing drug. After 6 months, both groups experienced improvement in insulin sensitivity, indicating inositol may be just as effective as metformin for women with PCOS. This is an active ingredient in Sensitol. Berberine Berberine is an isoquinoline derivative alkaloid extracted from various Chinese medicinal herbs that has also been used as an insulin sensitizer. In a randomized controlled trial of 89 women with PCOS and insulin resistance, berberine treatment was compared with metformin for 3 months. It was found that berberine effectively improved body composition, lipid levels (which are often imbalanced in PCOS due to sugar dysregulation), sex hormone-binding globulin, fasting plasma glucose, fasting insulin, and insulin resistance. A meta-analysis and systematic review confirmed the same conclusion that berberine improves insulin resistance and glucose metabolism similar to metformin. Cinnamon Though not compared to metformin, cinnamon powder has also been shown to improve insulin resistance, glucose metabolism, and lipid profiles in women with PCOS. In a randomized double-blind placebo-controlled clinical trial , 80 women with PCOS were given 1.5 grams per day of cinnamon powder capsules for 12 weeks or a placebo. Improvements were noted in fasting insulin and insulin resistance in those taking the cinnamon compared to placebo. The clinical outcomes of PCOS, including infertility, severe acne, and hirsutism, are often devastating for women. Hormone balance to address hyperandrogenism is most often the focus of treatment, but as an increasing amount of research points to insulin resistance as an equally influential element of PCOS, a focus on insulin sensitizers can’t be ignored. Diet is a great place to start in rebalancing glucose, but it is often not enough. Inositol, berberine, and cinnamon can also provide the support needed to address insulin resistance in these situations. I personally prefer N-acetyl cysteine over berberine and cinnamon. Other effective nutritional suppements include reishi mushroom, green tea, and spearmint tea.

Chicken Liver Pate Ingredients 1 lb chicken livers (Bell & Evan’s Organic is my choice) ½ cup chopped white onion or shallots 2 Tbsp grass-fed butter 1 tsp allspice (or nutmeg) ¾ tsp salt ¼ tsp black pepper 1/3 cup bourbon (can substitute red wine, or other alcohol, or chicken broth) ¼ cup currants or raisins 1 Tbsp powdered gelatin 2 egg yolks (optional) 2-4 Tbsp grass-fed butter (for pureeing) Directions: Drain chicken livers. Sauté onion/shallots in 2 Tbsp butter for 5 minutes on medium heat, add allspice, salt and pepper and cook 1 minute longer. Add in chicken livers and sauté 10 minutes on medium-low heat, or until firm and cooked inside. Add alcohol or broth and currants/raisins, cover, and simmer on low for 5 more minutes. Turn off heat. Sprinkle on gelatin, wait 1 minute then stir in. Allow mixture to cool 15 minutes. Puree in food processor with egg yolks and additional butter until smooth. Transfer to serving dish and chill 6 hours or more. Serve with sliced French bread or crackers and pickles.

I was really excited to read about this study as I believe it can be very helpful to new moms who question whether they are producing adequate breast milk. In summary, breastfeeding mothers who took an herbal formula containing ginger, turmeric, and fenugreek saw an almost 50% increase in the quantity of breast milk produced after 2 weeks, and over a 100% increase in quantity after 4 weeks. These are remarkable increases which could be helpful if you (or someone you know) have concerns your baby is getting enough to eat. Below is the published abstract and link to the study. You can cook with these herbs, or alternatively, here is a link to products that you can combine to create a similar formulation: https://us.fullscript.com/p/stores/products/catalog/show?productID=76113 and https://us.fullscript.com/p/stores/products/catalog/show?productID=69220 . Please note that you will need to connect with me or another provider to order them here. Abstract Background : Exclusive breastfeeding is the best way to accomplish optimal growth and health in infants. Low milk volume is a major problem that leads to nonexclusive breastfeeding. Objective: This study aimed to examine the effects of mixed herbal supplementation, including fenugreek, ginger, and turmeric on human milk volume and nutrient content. Methods: The study design was a randomized double-blind controlled trial. Fifty exclusively breastfeeding mothers were randomly divided into two groups. The herbal group (n = 25) received mixed herbal supplementation containing fenugreek, ginger, and turmeric, three capsules three times daily for 4 weeks. The control group (n = 25) took a placebo. Anthropometric and dietary data, blood pressure, heart rate, and blood and milk samples were collected at baseline and 4 weeks after the intervention. Milk volume was measured using a manual breast pump and recorded for 2 days at baseline, week 2, and week 4. Results : Breastfeeding mothers receiving herbal supplementation had a 49% increase in milk volume at week 2 and a 103% increase at week 4. These increases were greater than mothers in the placebo group (p < 0.05). There was no difference in milk nutrient content for both groups. Moreover, there were no differences in adverse effects observed in the placebo and herbal groups. https://www.liebertpub.com/doi/abs/10.1089/bfm.2018.0159?journalCode=bfm

I have been experimenting with a meal kit delivery service. The one I selected is a bit of an upscale product, that includes a lot of organic, wild-caught, or more “natural” ingredients. One of my patients has been trying several of them and suggested this one for me, and sent me a coupon code for $40 for the first delivery (email me if you want to get your own $40 off!) I have received 3 deliveries so far. What I like about these MEAL KITS: My husband can now prepare rather tasty meals without me having to show him where the ingredients are in the fridge etc. or how to put them together. He seems to enjoy the process as well as it takes away any guesswork. Great when I am working late to come home to a fresh cooked meal! The proteins that come in the kit are more than adequate in portion size and are very fresh. The sauces and seasonings are very tasty and the amount supplied is more than enough. The ingredients in the box stay cold on my front entrance-way for at least 6 hours. It is easy to order on the site and to select outside of the standard offerings. (Sun Basket) What I feels needs to be improved: The portions of vegetables are often smaller than I usually serve. Some of the produce is not quite as fresh or as ideal as I would choose. Sometimes an ingredient is not what I would have selected (non-pitted vs. pitted and chopped dates for example). The instructions for preparing the meal aren’t always how I cook. For example, one recipe said to put chopped shallots into the water for cooking the farro grain; I changed this by simply mixing them into the sliced fennel that I oven-roasted which to me resulted in more flavor. In about 1 of 3 meals, I don’t find the total amount of food to be enough to satisfy my hunger and the way I normally eat. What will stop me from using this service more often: The amount of disposal and/or recycling of packaging materials. The high up-charge for premium fish (when I chose halibut instead of salmon). All of the proteins are boneless and skinless, so they’re missing the collagen source (see my book on why this is so important). Cost is relatively high at between $25 and $30 for 2-serving meal. But less money and time than eating similar gourmet meals out. How I have modified some of the meals: I open the kit in the morning, and soak all my grains in water at room temperature to help them cook faster and be easier to digest. I often add an additional carb source, for example, I added sprouted quinoa (cooked) to the spicy lamb, carrots and kale meal which made it quite satisfying. I throw in a little extra baby spinach or other green when I think the amount of greens is a bit skimpy. Why YOU might want to try one or more MEAL KIT DELIVERY SERVICES: You really are new to this whole “cooking” thing. You want to develop your own repertoire of fairly easy and quick recipes that are your weekly “go-to’s.” You really hate grocery shopping or don’t have time to do it. You want more control over what you are eating and know that you are getting the right amount of protein, carbs, and calories. You are in a rut and just want to switch things up a bit. This is what I have gained from this experience. You live alone and need a reason to cook for yourself! So I say go for at least one order (a value with the $40 off!) and see what you think!

Eggshell Membrane– a Collagen Source that is not Just for Vegetarians In my book, I noted that all collagen products were derived from animal sources and as such, a true vegan/vegetarian collagen supplement was not available. I was not entirely correct. Yes, all collagen products are from animal sources, but not all are derived from living animals. There is one kind that comes from a chicken egg – as the title of this blog says eggshell membrane, ESM for short. So, if someone is an ovo- or lacto- ovo-vegetarian they could choose to take an ESM supplement, but of course a strict vegan or lacto-vegetarian would likely not. Nor could a person with an egg or egg white allergy. Yet perhaps the more important question is why choose to take an ESM supplement – what benefits could one expect? To answer this question, an understanding what ESM is would be helpful. Eggshell membrane is the thin membrane that lies between the hard eggshell and the “fluid” white of a bird’s egg. It is isolated from chicken eggs and contains not only a lot of Type I collagen (as well lesser amounts of types V and X), but also glucosamine, chondroitin, glycosaminoglycans, and hyaluronic acid. These biological compounds have been studied separately for their positive effects on joints. The fact they are all combined in one naturally-derived supplement is pretty amazing A few studies have been conducted on humans using ESM, in the form of a product called Natural Eggshell Membrane (NEM®). NEM is partially hydrolyzed through a patented enzymatic process similar to ones used for other high quality forms of collagen peptides. It is available in vegetarian capsules. The studies were sponsored by the product manufacturer, ESM Technologies LLC. In all studies, a daily dose of 500mg of NEM was taken with water before breakfast. Participants were required to discontinue all prescription and OTC pain relief medications before and for the duration of the study. They also were not permitted to take joint-targeted supplements such as glucosamine or chondroitin sulfate. In the first smaller pilot study, five adult women and six adult men, all seeking relief from persistent painful joint and connective tissue conditions, were enrolled. There was no control or placebo group. In this study, the participants had a 43.7% increase in flexibility, a 72.5% reduction in general pain, and a 75.9% reduction in range-of-motion-associated pain. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2697588/ In a second study reported in the very same publication, 28 subjects, six male and 22 female, again with various joint and connective tissue conditions, were enrolled. Fourteen were randomly chosen to receive NEM-Y and similarly 14 received NEM-X (two different ESM formulations). There was no placebo group. Twenty of the 28 participants completed the one-month study. Results were compared to the baseline at the time of entry into the study. Both treatment groups experienced a significant reduction in pain (NEM-Y 31.3% and NEM-X 18.4%) after one week, so the “Y” group was switched to the same NEM-X supplement. After 30 days, the mean reduction in pain was 30.2% for the combined X and Y group. The report did not detail the differences between the X and Y products. Considering both of the above studies, a significant proportion of the study populations (64% in the smaller group and 35% in the larger group) experienced a greater than 50% reduction in pain after 30 days. These two studies were small and “open-labelled” which means that both the researchers and the participants knew who was taking what, and there was no control group that took a placebo. From these initial investigations, NEM appears promising, but as any good researcher would state, “more studies need to be done.” Indeed, a few other promising studies have been conducted with NEM, and I will comment on the most recent one below. A third more extensive study was recently published in 2018, again conducted by ESM Technologies. In this placebo-controlled randomized trial, 30 post-menopausal women were given NEM and 30 received a placebo. Similar to the first two studies, the researchers measured changes in exercised-induced joint pain or stiffness. Additionally, they measured changes in cartilage turnover induced by exercise, using a urinary marker called C-terminal cross-linked telopeptide of type-II collagen, or CTX-II for short. Elevations in CTX-II are seen in osteoarthritis and rheumatoid arthritis, but also in healthy individuals including college-aged cross-country runners who put considerable stress on their joints. Interestingly, college swimmers and rower do not show elevations in urinary CTX-II, which is not unexpected due to the low-impact nature of their sports. Postmenopausal women have twofold higher levels than age-matched premenopausal women. This study of 60 post-menopausal women was a little different than the first two studies in that it measured changes in pain (and CTX-II) following the performance of a “stepping” exercise regimen every other day. Supplementation with NEM resulted in significant reductions of urinary CTX-II after one and two weeks of exercise, to levels below those measured at the onset of the study. After the two weeks, the amount of pain the NEM group experienced immediately following exercise was 38.1% less than the placebo group, however this was not statistically significant. Most notably, at the end of the two weeks, “recovery pain” (pain experienced immediately following and 12 hours after exercise) had nearly returned to “resting pain” levels for the NEM group, while the placebo group had levels of recovery pain that remained significantly higher. A similar effect was observed for recovery stiffness between the two groups. The researchers attributed the improvements in the NEM group to a proposed reduction in proinflammatory compounds called cytokines, which are released by the body in response to physical stress. They also suggested that the NEM has an immune-modulating effect and noted that half of those diagnosed with progressive osteoarthritis experience immune-mediated collagen degradation. My suggestion is if you are experience joint pain with physical activity, and after a couple of months of a joint-targeted collagen supplement with the addition of glucosamine sulfate, chondroitin sulfate and MSM, and perhaps turmeric or bowellia extracts, you still have pain or stiffness, you may want to try eggshell membrane collagen. If you want to try this at home, you may want to start saving your empty egg shells and drop them into your broth as it simmers for the last couple of hours. Just be sure to wash them before you use the eggs as the outside may harbor harmful microbes. You can store them in the freezer as you collect them, and then soak them in apple cider vinegar which will help release the calcium into your broth. I used to do this but fell out the habit – but after this article I will definitely be trying this at my home again!

I am sharing press release below because I thought it would be very helpful for many of my patients. (Original source: https://www.eurekalert.org/pub_releases/2018-12/uoca-seo120418.php ) DHEA is an OTC supplement used by many people as they get older. You would want to ask your doctor to order a blood test for DHEAs and then supplement accordingly. Also, please consider collagen peptides and calcium collagen chelate supplements if you want to keep your bones strong – I go into detail about these in my book: The Collagen Diet, Rejuvenate Skin, Strengthen Joints and Feel Younger by Boosting Collagen Intake and Production: http://womenandfamilynutrition.com/about-the-book/ Sex-specific effects of DHEA on bone mineral density and body composition Among older women, the naturally occurring hormone DHEA may preserve bone and muscle mass when compared with placebo, study suggests. University of Colorado Anschutz Medical Campus AURORA, Colo. (Dec. 4, 2018) – Women 55 and older have an increased risk of bone and muscle loss but therapy with the hormone Dehydroepiandrosterone (DHEA) may help prevent bone loss and increase muscle mass in older women , according to a new study led by Catherine M. Jankowski, PhD, FACSM, an exercise physiologist and associate professor at the University of Colorado College of Nursing at the Anschutz Medical Campus. The study was published last month in the journal Clinical Endocrinology and highlighted in Endocrinology Today. Jankowski and colleagues analyzed data from four single-site, double-blinded, placebo-controlled, randomized clinical trials sponsored by the National Institute on Aging designed to assess the effects of oral DHEA therapy on bone mineral density (BMD) and body composition in women and men between the ages of 55 to 85 who were not using sex hormone therapy. The dose of DHEA used in the studies increased circulating DHEA sulfate levels to that of young adults. “Because age-related decreases in androgen and estrogen production contribute to the loss of bone and muscle mass in older adults, restoring DHEAS to youthful levels may be an effective strategy for maintaining bone and muscle,” said Jankowski. In all four studies, dual-energy X-ray absorptiometry (DXA) was used to measure total body fat and lean (muscle) mass, and bone mineral density of the proximal femur, total hip, and lumbar spine at baseline and after 12 months of DHEA or placebo administration. Serum DHEA sulfate, estradiol, testosterone, sex hormone-binding globulin and insulin-like growth factor I concentrations were also measured at baseline and at 12 months. Researchers merged data from the four studies into a central database and compared the 12-month changes in BMD, body composition, circulating hormones, and growth factors in response to oral DHEA therapy versus placebo. Of the 486 cases, 138 women and 98 men had low bone mass, and 29 women and 11 men had osteoporosis. The researchers found that DHEA therapy was associated with increased BMD of the lumbar spine, total hip and trochanter in women, but not in men. The increases in BMD in women were not as large as seen with other treatments such as bisphosphonates. “Unlike some pharmaceutical trials targeting BMD, the DHEA trials we conducted did not target women with osteoporosis, which may have contributed to the modest increases in BMD,” said the researchers. “It is possible that DHEA therapy could be a strategy to mitigate the decline in BMD in postmenopausal women who do not tolerate other treatments,” according to Jankowski. However, the authors also concluded that the safety of long-term DHEA therapy (more than one year) needs further research. The investigators also found sex-specific results effects on fat-free mass (which includes muscle mass) in women and a decrease of 0.4 kg fat mass in men. None of the four trials controlled for exercise behaviors, which could have contributed to the increase in fat-mass of women taking DHEA. “Combining DHEA therapy with resistance exercise that imparts mechanical strain to bone may promote greater increases in muscle mass and BMD compared to either intervention alone,” stated Jankowski. “The beneficial effects of DHEA replacement on body composition are to modestly increase fat-free mass in women and decrease fat mass in older men, a reversal of the usual age-related trends in muscle and fat.” Jankowski and colleagues are currently conducting a randomized placebo-controlled trial to determine the independent and combined effects of bone-loading exercise and DHEA on BMD and muscle mass in postmenopausal women with low bone mass or moderate osteoporosis (NCT# 03227458).
Osteoarthritis is a painful condition that the majority of us will develop to one degree or another as we get into our senior years – and often sooner with an athletic injury. Besides pain, arthritis can cause a loss of physical function and lead to reduced muscle mass and strength. When physical activity is limited because of arthritis, conditions like diabetes and heart disease are much more likely to develop. Currently, there is no medical treatment than can slow down, much less reverse, the joint damage from arthritis. The standard of care focuses primarily on alleviating symptoms but medications prescribed for arthritis often have unwanted side effects. According to a recent review published in the journal International Orthopaedics, researchers have demonstrated that collagen protein supplementation can improve osteoarthritis symptoms. The review consisted of 5 separate randomized controlled trials published from 2009 to 2016, with a total of 519 patients. Treatment periods ranged from 10 weeks to 48 weeks. Treatment with collagen supplementation demonstrated a significant reduction of the total WOMAC index, a clinical tool used to assess the degree of arthritis (1) , and a significant reduction in stiffness and VAS score (a clinical “scoring” tool used to assess degree of pain) . The beneficial effects of collagen for the treatment and prevention of arthritis are not recognized by the conventional medical community. As described in my book, “The Collagen Diet,” collagen peptides that are broken into small fragments are the specific type of collagen that has demonstrated efficacy for a variety of degenerative conditions, including osteoarthritis and osteoporosis. When we ingest collagen peptides, they are further broken down into single amino acids and peptides consisting of 2-3 amino acids. These then enter the bloodstream and accumulate in joint cartilage (along with the skin, bones and other collagen-rich tissues.) In joints, the peptides stimulate the biosynthesis of cartilage by increasing type II collagen and proteoglycans that play an important role in the lubrication of cartilage. Hydrolyzed collagen peptides, rich in proline and hydroxyproline, can also promote an increased synthesis of hyaluronic acid from synovial cells. Decreases in both the WOMAC index and VAS score shown in this “meta-analysis” (2) demonstrate that collagen is effective for improving OA symptoms. Other potential benefits of collagen supplementation include improving skin elasticity and tone, sustaining muscle mass, supporting bone health, and blood pressure, and diabetes support. (1) The WOMAC consists of 24 items divided into 3 subscales: Stiffness (2 items): after first waking and later in the day Pain (5 items): during walking, using stairs, in bed, sitting or lying, and standing Physical Function (17 items): stair use, rising from sitting, standing, bending, walking, getting in / out of a car, shopping, putting on / taking off socks, rising from bed, lying in bed, getting in / out of bath, sitting, getting on / off toilet, heavy household duties, light household duties www.rheumatology.org/I-Am-A/Rheumatologist/Research/Clinician-Researchers/Western-Ontario-McMaster-Universities-Osteoarthritis-Index-WOMAC (2) A meta-analysis is a statistical technique used to calculate a (weighted) average of the combined studies. Cited study: Garcia-Coronado JM, Martinez-Olivera L, et al. Effect of collagen supplementation on osteoarthritis symptoms: a meta-analysis of randomized placebo-controlled trials. Int Orthop. 2018 Oct 27. doi: 10.1007/s00264-018-4211-5.

We love this easy recipe and so will your family! 4 servings Ingredients (just 3!) 4 Tbsp of unflavored gelatin 1 – 16 oz package of frozen fruit such as strawberries, mango, or peaches 1/4 – 1/2 cup sugar or honey (do not use honey if your child is under 1 year of age) In small saucepan, sprinkle gelatin onto 1/2 cup room temperature water to hydrate, then stir in well. After the gelatin has fully hydrated (3 to 5 minutes), add an additional 1 cup of water and heat on low until mixture is clear, but do not allow to boil. Stir in sugar or honey and cool for 10 minutes. (If using raw honey, you may want to wait until the gelatin/water cools to add.) Place frozen fruit in a blender. Pour cooled gelatin/water/sugar mixture into blender and IMMEDIATELY blend on high speed until fruit is completely pureed. You will notice that the mixture gets thick as the gelatin gets cooled by the frozen fruit. Pour into a serving bowl or into individual serving dishes. This “mousse” can be eaten immediately or put into refrigerator to keep for 3 to 5 days. Top with fresh fruit and yogurt or whip cream if desired. Nutrition information per serving made with strawberries and 1/3 cup sugar Collagen protein: 6g Calories: 125 Carbohydrates: 28g Fiber: 2.5g

Let me state up front that my book, The Collagen Diet: Rejuvenate Skin, Strengthen Joints, and Feel Younger by Boosting Collagen Intake and Production, was just released this week. (If you are interested in purchasing, please hop over to the “Where to Purchase” dropdown tab.) I also would like to share with you that before writing the book, I was on the fence about collagen supplements, even though a lot of my patients were consuming them even before their first visit. Collagen protein supplements, typically labelled as collagen peptides or hydrolyzed collagen, are the supplement du jour, close to taking over vitamin D in popularity. You may already be taking vitamin D for your PCOS and your general health (more to know about this that I discuss in depth here: https://www.westonaprice.org/health-topics/abcs-of-nutrition/vitamin-d-supplementation-panacea-potential-problem/ ). But are you taking collagen? I wasn’t until I did the research. Because of the scientific evidence, I am now convinced that including a source of collagen protein in a well-balanced diet is super important for many reasons. I go into these reasons in-depth in my book, but due to space limitations, I did not specifically address why collagen protein could be helpful for women with PCOS. And while collagen protein is thought of as trendy supplement, it is far from just that. It was historically a very important component of a nutrient-dense diet, part of the concept of nose-to-tail eating. But why might collagen protein be helpful for PCOS? It is known from a handful of studies that women with PCOS have lower levels of the body’s endogenous (that is, made in the body) master antioxidant and detoxifier: glutathione. One study showed cellular levels of glutathione were actually only half of those in women without PCOS. This goes hand in hand with the increased levels of damaging oxidative stress in PCOS, thought in part to be caused by higher levels of testosterone. High levels of oxidative stress are thought to underlie metabolic syndrome (marked by elevated blood glucose and dyslipidemia), infertility, and DNA damage. It is also a reason that women with PCOS are at higher risk for diabetes and heart disease. Unfortunately, it is suspected that this oxidative stress may be one of the reasons many women have difficulty managing this condition, despite good dietary and lifestyle practices. Enter collagen protein. Collagen protein is the second-best dietary source of glycine (edible bones are the best source, but not widely consumed!). Glycine is one of the three amino acids that the body uses to create glutathione, along with cysteine and glutamate. If three are needed, why single out glycine? Because glycine is often the limiting amino acid (meaning the one the body runs out of) controlling the synthesis of robust quantities of glutathione. The amount of glutathione the body can make is decreased if there is an inadequate supply of glycine. Studies cited in my book show that most people have a shortfall of glycine in their diets, by several grams per day. Studies also show that increasing the intake of glycine can increase the amount of glutathione made, and this can occur in a matter of a few weeks. My advice: a good rule of thumb would be to include 1-2 grams of collagen protein for every 10 grams of total protein eaten each day. So, if you are consuming 75-100 grams, typical for women between 125 and 175 lbs, that would be 7.5 – 20 grams. You can get this from a collagen peptide supplement, gelatin, bone broth, or fish and chicken consumed with the skin. You will find lots of other ways in my book and tips on what to look for in a supplement. One of the side benefits of consuming collagen protein/glycine is you may actually find your blood sugar becomes less erratic, your skin hydration improves, you sleep better, and you may even see your hair on your head get thicker and your nails stronger. For me, my HbA1c dropped by 0.5% with a regular collagen regimen which was an unexpected benefit. Finally, as detailed in my book, consuming low-temperature processed whey protein along with your collagen protein could improve glutathione levels even more than collagen alone. This is because there is a special form of highly bioavailable cysteine in this type of whey protein that also supports robust glutathione synthesis. I have a shake with whey protein, collagen protein, and plain kefir daily. If you are thinking this might be helpful for you, please discuss with your doctor or a knowledgeable nutritionist, and then choose your collagen supplement carefully (again something I cover in the book.)

Just made my first batch of “cool weather” bone broth and it turned out perfect! You can tell it is rich in collagen protein because it firmed up in the refrigerator (note the lump sitting on top), a property of the gelatin form of collagen protein. So below is what I did in a nutshell. You can find more detailed tips on making good bone broth and why collagen protein is so important for health in my book, The Collagen Diet: Rejuvenate Skin, Strengthen Joints, and Feel Younger by Boosting Collagen Intake and Product, just released this month! 10 steps to perfect bone broth: Buy the best bones you can find and include a mixture of marrow and knuckle bones that have a lot of connective tissue on them. I got mine frozen at a farmer’s market – pastured beef bones. Place bones in a lightly oiled heavy stockpot. I used a Le Creuset enameled pot with a bit of olive oil on the bottom to prevent the bones from sticking. Roast bones, uncovered, until medium brown in a 375-degree oven, about 15-30 minutes. I set my oven on convection roast however I needed almost 40 minutes because they were frozen when I started. I broke up any clumps as the bones began to warm so they would brown more evenly. Remove pot of bones from oven and add purified water to cover, or spring water as available. Bring to a gentle boil over medium heat, but do not put the lid on. Reduce to a simmer and continue cooking for 12-24 hours. (I cooked for 20 hours) Add more water as needed to keep the bones covered. If leaving unattended for any length of time, cover the pot so to limit evaporation. Using a slotted spoon, remove bones and allow bones to cool so you can handle them. I remove the bits of meat and connective tissue and save that for adding to soup or just eating – super good for you! Pour broth through strainer into a smaller pot that will fit in your refrigerator. Allow to cool at room temperature for 30 minutes or so. You can also transfer to heat-resistant glass jars, just take care that the broth has cooled a bit so not to risk breaking the jars. I add several ice cubes before putting warm broth in the fridge, if cool enough outside (less than 40 degrees and providing that no animals will get into it!) the broth can be placed outside to cool for a few hours or overnight before placing in fridge. Remove fat from surface and use broth in recipes for soup, grains, legumes, and even cooking vegetables like collard greens and kale. Stores up to one week refrigerated, the fat on surface will keep it fresher. If you want, you can scrape the broth off the fat chunks and pat the fat dry with a paper towel, place in freezer, and use for cooking: roasting potatoes, browning meat, making refried beans, etc.

“To get a period, you need to be fully nourished in every respect. That means enough calories and enough micronutrients such as zinc and iodine…” This quote comes from a book entitled “Period Repair Manual” written by naturopathic physician Lara Briden. It is one of a few books that I routinely suggest women read to get a better understanding of how to interpret their cycles. Why is your period more than just your period? Because it is a window to your overall health. It can also be a window to your overall nutritional health as Dr. Briden sums up so well. First and foremost we have to consider whether your body has assurances that there is plenty of food (calories) available to allow it to be fertile. Strange you may be thinking – perhaps you are like other women who have been told that losing weight could result in more regular cycles. Yet there is a balance between achieving appropriate weight loss and potentially under-eating. And although you may not be planning a pregnancy, having regular periods is a sign of good fertility which depends on overall good health. Beyond adequate calories, we need to look at several other key dietary factors. Certainly sufficient high quality protein is important, and while there is no one-size-fits all carbohydrate intake, it is not generally a good idea to eat too few or too many high carbohydrate foods. Micronutrients include not only the two minerals she mentions, but an array of essential vitamins and other minerals, more than 2 dozen are required in adequate quantities and just as importantly, in balance with the others. My mission is to uncover where you might be lacking in nutrients, and where you might be consuming foods or ingredients in foods that actually detract from your overall health and nutritional status. Going beyond diet, I then work to help you identify other lifestyle habits and influences that disrupt your body’s natural hormonal signals and put your periods out of whack. While I highly recommend “Period Repair Manual,” I don’t recommend women go it alone when trying to fine-tune their nutrional intake. It only takes one dietary imbalance to stress a women’s body and possibly disrupt the regularity of her cycle. Give me a call (919-800-0343) or send me an email (womenfamilynutrition@gmail.com) and let’s talk about your needs and goals. In the meantime, you can start reading Dr. Briden’s book for free: http://a.co/ho9vu6M

“I can’t stress this enough, I AM NOT DIETING.” Or so says a young woman who was profiled on the Rachel Ray show after she lost 180 pounds (350 down to 170 pounds) in less than 2 years. That represents about a 2-pound weight loss each week. What did she do to achieve this amazing weight loss? She ate only homemade unprocessed foods at meals. She exercised regularly instead of sitting on the couch. And she decreased her calories from 3,000-4,000 per day to 1,200. If 1,200 calories per day, day after day, is not a diet, then what is? Even the trainer on Ray’s show, Bob Harper, called her intake a “drastic reduction.” Her question for Bob was what was a good maintenance level of calorie intake? He suggested 2,000 calories per day as an appropriate long-term plan. This remains to be seen of course, and he added that she should keep tabs on her weight on a weekly basis to see if the 2K estimate was a good one. I hope they follow this young woman over time, as it will be interesting to see what happens when she begins to eat 2,000 calories per day. I wish this woman well, but my suspicion is she will immediately begin to gain back some weight, how much is hard to say. Think about this, she has stopped losing weight, or at least slowed down considerably at this point. This is a good thing because her body, just like everyone else’s, knows how to protect itself from wasting away when food is scarce. Otherwise, she could theoretically just keep losing weight until she was skin and bones. Of course, she could waste away eventually, but she would probably have to decrease her calories even more now to have this happen. The human body is very smart and knows how to adapt to very low food availability. What point am I trying to make here? Well there are a few important takeaways from her story. First, 1,200 calories per day for an active woman IS A DIET, no matter how high quality the foods eaten are. Second, this is a highly unusual outcome – to steadily lose this much weight without hitting at least one plateau. It is very likely that this woman had not dieted before, at least not on a regular or protracted basis. Third, exercise is just as important as food to help preserve muscle mass – and she did look pretty fit healthy even with the advantage of being in her 20s. Finally, fourth, DO NOT TRY THIS AT HOME! You do not want to risk melting down your metabolism, which is almost a guaranteed outcome of this type of weight loss. I repeat, you do not want to put yourself in a metabolic state where your body has adapted to consuming a very low-calorie diet. If you do, there is a strong probability that you will struggle with maintaining an ideal body weight for perhaps the remainder of your life. If you are experiencing difficulty losing weight, consider how many times you have been on a diet. If more than a half-dozen or so, your body has adapted to a low-calorie intake to some extent. This does not mean it is impossible to get closer to your goal, but it is not easy. Don’t let anyone tell you otherwise – fast weight loss equals fast weight regain. (If you have not been chronically on a diet, several other factors may be in play which can be uncovered with a good nutritional assessment). What can you do? Don’t give up hope, give me a call to see what I can do for you. I cannot promise that you will reach the weight you were in your 20’s, but I can help you get healthier and fitter and have more energy – all things that must happen before you can lose fat and keep it off for good.

I can be Debbie Downer Dietitian at times, spoiling everyone’s food fun. At the same time, I will be the first to admit that I do not follow my own “food rules” 100% of the time and I don’t expect my clients to do so either. So now that we are heading into outdoor cooking and eating weather, what is my advice on grilling food – healthy or not, or somewhere in-between? And what do I do personally? Short answer: limit or avoid grilling, especially if you have a metabolic health problem. Long answer: you can make grilling food healthier by taking a few simple steps. But still a good idea not to grill too often – I generally eat grilled food less than one time per week in the summer. Why grilling meat and other animal protein is harmful. It is because all browned meats develop toxic DNA-damaging compounds called heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs), which are strongly linked to an increased risk for cancer. The higher temperature used for cooking and the darker brown and even black they become, the greater the amount of HCAs and PAHs that are created. Grilling temperatures are typically the highest of all cooking methods, and the food is more likely to get very dark on the outside, increasing the toxins in the foods. But even pan-searing can create an undesirable amount of these toxic chemicals. Meats, especially fatty meats, will develop the highest levels due to the heat and flame generated when the fat drips onto the heat source of the grill. Leaner proteins such as chicken and fish are usually less problematic. Maybe this is one reason we are advised that red meat is linked to cancer? Besides never grilling again, what can you do? First and foremost, use the lowest grill temperature that gives you the results you want. Beyond that, here is good evidence that marinating your protein foods in an acid-based marinade for a couple of hours can substantially reduce the amounts of HCAs and PAHs. (I have included links to recipe ideas below). You will also want to add herbs to the marinade, for example rosemary and garlic to a lamb marinade, as this can further reduce the quantities of toxins. Avoid brushing on sweet-tasting barbeque sauces, the sugar in them increases the formation of toxins during grilling. It can be a good idea to pre-cook meat at lower temperatures in the oven and then finish with a brief grilling. Turning meat frequently also helps as the temperatures won’t get quite as high on the surface. Finally, if you like grilled chicken, here is one time I would advise you to remove the skin before grilling as the fat under the skin can increase the browning of the chicken. Save that skin for your chicken soup. What about vegetables – grill or not? We know that starchy foods develop a known carcinogen called acrylamide when fried or baked – an indication again is how brown they turn. Because vegetables are moister and have substantially less protein (which is part of the undesired reaction) grilling vegetables is not generally considered a problem compared to meats and poultry. But still, avoid letting your vegetables get more than just a medium brown to be on the safe side. What else should you eat when you do choose to eat grilled meats? Broccoli to the rescue! Compounds found in vegetables in the cabbage family help block the damage that HCAs and PAHs do to our DNA, but they can’t completely prevent it of course. This is where a nice lemony-vinegary-cabbage-broccoli slaw comes in. Not only a good balance of flavors with a heavier meat entrée, but protective of your health at the same time. And if you are really want the most protective veggie, include a salad made with arugula or watercress and perhaps a handful of broccoli sprouts. Tips to make a marinade for grilling meats: https://articles.mercola.com/sites/articles/archive/2014/07/19/grilled-meat-carcinogens.aspx References for additonal reading: http://www.washingtonpost.com/wp-dyn/content/article/2008/08/22/AR2008082201119.html http://www.foodandwine.com/news/add-spice-your-grilled-meats-make-them-healthier https://www.rodalesorganiclife.com/food/healthy-grilling

Just read an interesting news story about a recent study that looked at three popular weight loss diets: https://www.nutraingredients-usa.com/Article/2018/03/06/Study-reveals-micronutrient-gaps-in-three-commercial-weight-loss-diet-plans?utm_source=copyright&utm_medium=OnSite&utm_campaign=copyright No surprises there for me – the study confirms what I see daily in my practice. People who follow weight loss diets put their overall health at risk when they don’t seek proper nutritional guidance . You may think – simple to solve, just take a vitamin. Good idea, but consider that while many health-conscious dieters do take a supplemental multivitamin, I find that most do not select one that is actually the best match for their needs. Often selections are made based on cost, convenience, or the desire to take as few capsules or tablets as possible. Even people who choose more pricey supplements may not fully appreciate the differences in product formulations. (I often compare understanding nutrition to understanding the US tax code – which is why I trust and rely on my accountant to do my taxes!) Consider this: a superior quality vitamin generally costs less than $1 per day, and an even more comprehensive supplement regimen may only equal the price of a single Starbucks beverage or an after-work beer. But outlay is only half the equation. The most important cost benefit is the results: my patients typically report increases in energy, reduction in hunger, less frequent colds, and improvements in sleep (among other things) when the missing nutrient needs we identify are consistently met. You may think, well if a diet was well-designed, certainly I could get everything I needed from food. Maybe yes, maybe no. A well-designed, well-balanced diet would include things like organ meat, seafood, bone broth, fermented foods, properly prepared grains and seeds, grass-fed dairy, meat, and eggs, and of course a few helpings of fresh fruits and vegetables daily. Do you have to eat like this to be healthy? No, but it is the best way to ensure that you are meeting all of your nutrient requirements – both macronutrient and micronutrient (vitamins and minerals). For myself, I typically come close to that way of eating (organ meats present a challenge mostly due to availability), but find that I still feel better when I take certain supplements on a regular basis, including a multivitamin, highly absorbable minerals, a few food-based products, a supportive herb mixture, and functional nutrients like coenzyme Q10 and inositol. Is the cost worth it? I think so, but the only way to really know is to first follow the most nourishing diet plan you can, get a review of any potential nutrient gaps, and then add in a targeted supplement plan that is carefully matched to your needs. A well-designed supplement plan, together with the most nutrient-dense diet you can consistently follow is an investment in your health and the quality of your life. Don’t risk it – your body is amazing but can’t go on indefinitely lacking even a single nutrient without showing some signs eventually. Get the guidance of a qualified nutritionist – your body is the most important asset you will ever have!

During this unusually cold North Carolina winter, many of my clients are coming in with upper respiratory infections; some have rescheduled their appointments because they have either very bad cold or even worse, the flu. For those of you who are suffering with a seasonal virus, I wish you a quick recovery. But beyond wishing and praying, there is more that you can do to protect yourself from what often seems to be another inevitable downside of winter. I am blessed to be able to tell you that over the past 17 years, I have had 3 viral illness: 2 colds and 1 stomach bug (which may have been food poisoning). Prior to that 2000, I recall that I generally got at least 1-2 colds per year, almost always occurring between January and March, usually following a time when I became a bit run down. I don’t remember having the flu in at least 25 years, and have only taken the flu shot one time, about 20 years ago before our family went on a ski trip to Canada. So what am I doing differently so I don’t come down with even one cold each year? First and foremost, I believe it is my vigilant practice of getting optimal amounts of the fat soluble vitamins, especially vitamins A and D. Vitamin A and D work synergistically, neither alone is as effective as their combination to support the immune system. Research from the mid-1900s clearly demonstrated they were much more effective (and safe) when taken together in relatively robust doses. Back then, there was greater interest in preventing viruses nutritionally because so few drugs were available. After discovering the work of Weston A. Price in 2000 ( www.westonaprice.org ), I realized that optimal sources and quantities of vitamins A & D were missing from my otherwise pretty nutritious diet. So besides eating beef and chicken liver periodically, I began to supplement with vitamins A & D from fish liver oils and/or vitamins that contained pre-formed vitamin A (retinol, not carotene) along with vitamin D, in amounts of 10,000 IU and 1,000-2,000 IU per day, respectively. I do believe plenty of vitamin A and the right amount of vitamin D is the number one reason I don’t get sick. I take extra if I feel I may be at risk for getting sick – up to 50,000 IU of vitamin A and 10,000 IU of vitamin D for a few days, always with a meal that has fat for best absorption. However there is more that I do if I began to feel that little “off” feeling – you know when your body is just a bit achy, you have a slight headache, your energy levels dip; in short, you just don’t feel like yourself. Please read on. Another way to support your immunity through your diet is chicken soup. I eat a lot of this in the winter anyway, but if my appetite drops due to feeling off, this is one food that almost always appeals to me. I prefer making my own chicken stock – using organic chicken legs and wings and necks when I can get them. I start the soup by placing the chicken parts in a large enameled pot, covering with filtered water, and simmering for 1 hour. Then I take out the parts, remove and refrigerate the majority of the chicken meat, and return the bones and skin to the pot to simmer for another 4-8 hours. I then strain the soup into another pot after removing all pieces of bone and skin, and put outside to cool initially, then into my fridge. I skim the fat, reheat with my desired vegetables (celery, carrot, garlic), add back the cut-up chicken, then cook rice or noodles directly in the soup. I season with salt, poultry seasoning or sage, and parsley. So good and so comforting. Make sure you make a big pot! If you don’t have time to make broth, try Swanson’s Organic Bone Broth in chicken flavor, or another brand that you like. I find the Swanson’s product is pretty tasty and is actually made with the chicken bones, unlike some of the other types on the market. (I have tried some of the other bone broths on the market, and some are pretty tasteless unfortunately.) Here is a list of what else seems to be working for me. This self-care protocol is based on both my research and my own experience, but please keep in mind it is not a medical treatment that takes the place of your healthcare provider’s evaluation and treatment. One, I take more supplemental vitamin C, so instead of the 300-500 mg I take generally each day (along with raw fruits and some raw vegetables), I will take 2-4 more 500 mg capsules of an high quality, professional brand, spread throughout the day. Two, I take AHCC, activated hexose correlated compound, three 500 mg capsules on an empty stomach twice a day, in the morning and at night. These work to activate the first line defenses in the immune system and they are pretty amazing overall for this purpose (and other applications like cancer support – always check with your doctor if you have cancer, an autoimmune disease, or other serious medical diagnosis). Three, I take Life Extension’s Enhanced Zinc Lozenges ( enhanced zinc lozenges ). This is a tip I learned from Chris Masterjohn, PhD. There are a lot of types of zinc designed for viral protection, but I think this formula has proven much more effective than almost anything else on the over-the-counter market. I generally take 2-5 per day, allowing then to slowly dissolve in my mouth to maximize efficacy. I only take for up to 7-10 days, so not to consume too much zinc which can be a long term problem if you are not zinc deficient. A bit chalky, kind of large, with a somewhat metallic taste – so while you may not enjoy them, they are certainly more enjoyable than getting sick. Four, I take elderberry syrup, a teaspoon or two 2-3 times per day for the duration of my feeling slightly under the weather. This is a very old-time remedy that does have some scientific backing. This is great for children as the flavor is like an intense grape jelly so most will accept taking it. Store in the refrigerator after opening and don’t let your children drink out of the bottle! Fifth but not least, I take a good garlic product that is supportive of immunity; this is something you can use longer-term if you wish. Garlic can be taken in capsules, but make sure you get a high-allicin product ( optimized garlic supplement ). If you choose to use whole garlic cloves, make sure you chop them finely, let them sit for 15 minutes to develop the active allicin in them, and mix into honey so they don’t irritate your throat or GI tract. Some people cannot tolerate raw garlic at all, so for them, capsules might be best. And of course, never give honey to a child less than 1 year old. I hope you and your family get through this wintry weather without just a few minor sniffles. But if you do get sick, you may want to try some or all of the above after a visit with your doctor when needed. In the meantime, stay cozy and remember NC winter’s pass pretty quickly!

To all of my patients who are taking a couple of weeks off from their dietary intentions: it’s okay, you are normal, and yes, there are a few things that you can do to make that January weigh-in less disappointing. When you are doing holiday feasting, guilt is a non-productive emotion, so please, please, let it go. To be perfectly honest, I must admit that I relax some of my usual healthy eating habits during times of celebration, and extended celebrations like the Christmas to New Year’s week are no exception. And I do enjoy it – with no guilt whatsoever. For me, the winter pounds almost never exceed 5 additional from my usual weight. I do believe my well-nourished body and relatively active lifestyle helps keep weight gain to a minimum, but I want to share with you some tips that both experience and science show do work. First of all, mindful eating is super important. In a pecan pie nutshell, this means really enjoying the food you eat, savoring each bite and letting go of any regrets that you actually ate a second piece of pie. The important thing is to EAT SLOWLY so the pleasure you get from each bite is maximized, and your body has time to recognize the calories you are eating. Many of my patients admit that eating fast is something they struggle with, often because they feel they need to move on to the other tasks on their proverbial plates (me too!). Taking an additional 10 minutes to finish a meal is probably not going to adversely impact your overall schedule, and an added bonus is that any tendency to bloating could be reduced by thoughtful chewing. Many patients have told me this simple change makes a huge digestive difference and helps them eat less because they become too full to take seconds. Second, at gatherings outside of your home, survey the options before taking a helping from all. Start with mix of foods that will fill you up – especially PROTEIN foods like turkey, roast beef,or ham, along with green vegetables: esp. salads that are not doused in dressing or my personal favorite, Brussels sprouts; then take small helpings of your chosen favorites – such as sweet potatoes, stuffing, and creamy offerings – limiting these to 1/3 of your plate. If there are after-meal desserts you have your eye on, keep in mind that choosing one less of the carb-rich side dishes may be good strategy. Careful though if you have blood sugar issues – your portions may need to be 1/3 or less of what other might consider “normal.” Third, soup is something that we all should eat more of, not only if you are trying to keep your weight under control If you have been following nutrition trends, it would have been hard to miss the hoopla about “bone broth” and its myriad of almost miraculous benefits. It has been shown to enhance skin, joint, and blood vessel integrity, and some studies show that the collagen protein it contains can help with weight loss! I too am a big fan, and never miss an opportunity to use a turkey carcass to make a post-holiday soup. But getting good bones to make broth can be a challenge at other times. To get the weight loss benefits of soup, it is best to start with a slow-simmered bone broth, add a lot of vegetables, and at least 1/4 cup of cubed meat or poultry per serving, and eat before the rest of a meal. I recently tried a boxed form of bone broth that I actually found pretty tasty – Swanson Organic Bone Broth (chicken flavor) that I purchased at the Fresh Market. It has a decent amount of collagen and the list of ingredients is pretty clean. Use it to make a “homemade” soup, tossing in leftover chicken/turkey and vegetables, or frozen veggies and cubed raw chicken if your fridge has been cleaned out. I like to keep boxed broth on hand in case anyone comes down with a case of sniffles. (My next post will be on what to do when you feel the beginning of a cold coming on.) Finally, get yourself outside for a good brisk walk! Successful weight losers exercise daily for at least 30 minutes. The science behind exercise for weight loss is complex, but most of the benefits are realized in the first 30-45 minutes. Last night my hubby and I took a power walk at 6:00 p.m. and the crisp air, along with the beautiful holiday lights really lifted our spirits. By the end of the 2.5 mile walk, we were feeling quite warm despite the 40 degree temperatures. When we lived in New Jersey, we used to walk in snowy weather, often below 20 degrees, and I fondly recall the way it made us feel more alive. Just be sure to put on a warm hat, socks, shoes, and gloves before you go. What to do if you do gain a few pounds, especially after working so hard to take them off? First, don’t panic. Second, get right back on track because the longer you keep on weight, the more the body recognizes it as your “normal” weight – making it a little harder to lose in the future. Developing a consistent habit of getting back on track and staying there will make those holiday excursions less anxiety-provoking because you have experience resuming your healthy eating plan. See you in January!

Just yesterday I received an email from the Centers for Science in the Public Interest (CSPI) strongly criticizing the Trump Administration for their planned policy to remove childhood obesity from this list of federal priorities, and shift funding by the Centers for Disease Control (CDC) away from chronic disease prevention. With this, they requested support for their effort to speak out against this policy change.

Do you ever feel that your husband can pop out of bed more easily than you do? I certainly do. (Although when we were both undergrads at the University of Maryland, I seemed to always make my 8 a.m. labs, while he struggled to get to his occasional 8 a.m. class). Read on to find out why. Several years back, when I was attending one of my first integrative health conferences, I recall an interesting admission that a presenting medical doctor made. She was speaking on the topic of stress management, and was emphasizing the importance of getting plenty of sleep (and no, not just on the weekend!) She casually mentioned that she went to bed between 10 and 10:30 p.m. and woke up between 7:30 and 8:00 a.m. A whole 9-10 hours of sleep each night! And I thought I was being indulgent by sleeping 8-9 hours most nights, staying in my cozy bed until the kids got up around 7, while my husband awoke each weekday at 6 a.m. to catch a train to NYC. I instantly felt a lot less guilty about my extra winks, figuring, well if a busy MD does it (and she was an expert on women’s lifestyle and health), well so should I! Now that I work with women of all ages, I have noted a few things about women and sleep. One, they often get less than 7 hours, and many get less than 5-6. Two, quite a number of the very health-conscious women I see often will arise at 4:30 a.m. to make a 5-6 a.m. exercise class; not just once a week, but a few times a week or even daily. And three, almost all women feel they don’t have time to sleep longer (unless retired and no kids at home), and that more sleep would be nice-to-have, but not a health necessity. If you are not yet a patient of mine, I am going to give you some very, very important advice that I give my patients. Sleep is as important as a nourishing diet. No ifs, ands, or buts about it. The women who are able to follow my advice to skip a couple of exercise classes a week and sleep in, usually meet their health/weight goals more quickly than those who chronically short-change their shut-eye. Your body will be in a constant state of stress if you don’t get the sleep you need, and you can neither exercise or eat your way out of it. So back to the men vs. women thing. It is actually a scientific observation that women need 20 minutes more sleep per night, on average, than men. And guess why they think this is so? Well, we generally utilize more of our brain, in part due to our propensity to multi-task (anyone do that?) over the course of the day. So that makes us more tired. The human brain uses 20% of the body’s basal energy needs, more than the heart, the lungs, or even the muscles. Unfortunately, that doesn’t mean we can “think” our weight off, but it can mean that when we get tired from brain work we often crave a high starch or high sugar snack to replenish the brain’s supply of blood glucose. Anyone like me crave a carb (mine is a piece of fruit or bread with butter) after a long session of mental effort? Another problem I see is women struggle with their quality of sleep. Usually this affects women during the pre-menopausal through post-menopausal years, but can negatively impact women of any age. The more responsibilities, often the less sleep, especially when a woman has a hard time letting go of her to-do list or has a difficult life situation or challenge. Some women, like myself, were great sleepers until they had kids, and just around the time they started getting better sleep, perimenopause set in. One thing I do is investigate all the obstacles that stand in the way of good sleep. A few real patient examples: one woman stopped her diet orange soda, and switched to flavored seltzer, and was able to sleep without waking for the first time in many years. (Diet soda has aspartame, a brain excitotoxin as well as caffeine in some brands – her favorite had both.) Another woman was eating most of her daily protein at dinner, once we switched this to lunch, sleep was much improved and she was less thirsty at night as well so she did not need to wake to urinate as often. What’s preventing you from getting the sleep you need to live your best life? There is an answer, let me help you find it.
A recently published study pointed to an increased risk of worse outcomes when a women has an elevated glucose response, even when it does not meet the diagnostic criteria for outright gestational diabetes. I have spoken about this in the past on the late Dr. Su’s podcast (no longer available unfortunately).

A problem I frequently encounter in my practice is children turning their noses up at all vegetables, perhaps with the exception of raw (not cooked!) carrots. Parents feel this is really not healthy for their child, and to some extent, I would agree. However, raw fruit can cover a lot of these bases, so feel good about that if your child will eat at least 3-5 different fruits in the amount of 2 or more per day. I am not going into all the nutrients that vegetables provide, but I will address a few. They are a source of the vital mineral potassium, one that is in short supply in most of our diets. Potassium is especially important to balance our sodium (salt) intakes, as they are complementary nutrients, working to balance each other’s effects. Some experts feel higher sodium intakes are not a problem as long as they are accompanied by good intakes of potassium, and I would concur. Fruit is an excellent source of potassium, and an excellent source of vitamin C when eaten raw or very lightly cooked. You can also get a lot of “phytochemicals” from deeply colored fruits like berries; these play antioxidant roles in the body. But should you resort to preparing vegetables in any way that will get your child to eat them? That was the suggestion of Rachel Ray today on her television cooking show. She was making tempura with her guest Carla from “The Chew.” Rachel said “If your kids hate vegetables, put some batter on them and fry them.” This poor nutritional advice was made even worse by Carla’s recommendation to use vegetable oils, canola, sunflower, rice bran oil, to fry them in as they have a higher “flash point” – I think she meant “smoke point.” This is actually not completely true: https://whatscookingamerica.net/Information/CookingOilTypes.htm (To her credit she did recommend refined coconut oil – much better choice, but a pretty expensive way to fry.) What is wrong with this advice? Foods fried in industrial seed oils are some of the worst foods for health, foods I recommend my clients limit because they contain numerous dangerous by-products of highly-heated polyunsaturated fats. A great article to read on this: http://www.westonaprice.org/know-your-fats/the-big-fat-surprise-toxic-heated-oils / Some researchers feel that these industrial seed oils, a relatively new introduction into the human diet, are at least in part responsible for the obesity epidemic, the increase in cancer, even the rise in blood sugar control issues. Fats become part of our cell membranes, which are the “gatekeepers” of our body’s metabolic machinery. Hormones dock on the cell membranes, sending messages that regulate all aspects of our metabolism. If the docking sites are not operating at full capacity, we can may become slightly resistant to the effects of the hormones. The presence of “damaged” fats can also initiate oxidation chain reactions – leading to damage of cellular organelles, like the super-important mitochondria, which generates the majority of our body’s energy. Vitamin E in adequate amounts can help limit the damage, and vegetable oils are considered the best dietary source. However, the oxidation of fried oils will exceed the protective effect of any vitamin E that is present in the oil, so a net deficit of vitamin E actually can occur. So do your family a health favor, limit fried foods, and if you choose to fry, do so occasionally Try to use a more saturated fat such as beef tallow. I get my own tallow from the surface of beef bone broth I make. I lift it off when the broth is chilled, rinse with cold water, pat dry, and put in your freezer. Just be careful and heat slowly as the traces of liquid can lead to sputtering when you place it in your frying pan. Beef tallow has a high smoke point of 420 degrees, http://cooklikeyourgrandmother.com/how-to-cook-with-beef-tallow/ , which you should not approach if you keep the temperature around 350 degrees. If you don’t use a frying thermometer, just make sure the oil does not smoke, which means you let it get too hot. If your children like chicken nuggets and French fries when you go out to eat, try to limit this meal choice to 1-2 times per month. You can try making baked chicken fingers, a good recipe is here: http://www.recipetineats.com/truly-golden-crunchy-baked-chicken-tenders-less-mess/ . I often made something similar to these when my kids were young, using corn-flake or Panko crumbs and a mixture of olive oil and ghee, tallow, or palm oil to coat the pan (the recipe here says brown the panko crumbs in oil, I never tried that but may be a good idea.) Finally, good sources of vitamin E are fresh nuts and seeds, avocados, and cold pressed olive, sesame, coconut, and almond oils used in salads or in a lower temperature saute.

I wanted to share a short slideshow with those who are interested in learning why traditional nourishing dietary patterns help babies get off to the best start in life. Thank you to Fang, Dagmar, and Ken at Oriental Health Solutions, Durham, NC. http://www.orientalhealthsolutions.com/information/how-to-have-a-healthy-baby

Disclaimer: The following is meant for use as general nutrition educational content only. A woman, pregnant, breastfeeding, or trying to conceive, is strongly advised to discuss her need for vitamin A, or any specific nutrient, with her obstetrical/gynecological care provider. This is not meant to replace the advice of an individual’s qualified healthcare provider. I have written a detailed article published in the Wise Traditions Journal, Summer 2016 available at: http://www.westonaprice.org/health-topics/abcs-of-nutrition/fat-soluble-activators/the-scarlet-nutrient /. However, I realize that many of you may just want the “talking points.” So here they are: 1. Vitamin A is absolutely essential for the proper development and growth of a baby, before and after birth. 2. Vitamin A is now considered a nutrient to be avoided during pregnancy, largely based on one weak study and concerns about very large intakes leading to birth defects. 3. Most prenatal vitamins do not contain true vitamin A, also known as retinol, retinyl esters, or retinyl palmitate; some do contain beta-carotene, a vitamin A precursor. 4. Beta-carotene cannot meet the vitamin A needs of many individuals, whether from food or vitamin sources. Genetic variation largely accounts for this, but health status is a factor. 5. Liver is the best dietary source of vitamin A, around 3-4 oz a week will usually be sufficient to meet dietary needs, yet women are being advised not to eat liver. High quality cod liver oil is also an excellent source; traditionally both were consumed by pregnant women as late as the mid-20th century. 6. Vitamin A regulates cellular replication and the processes that cause a cell to become a certain type of cell to form tissues, such as a brain cell, a heart cell, a liver cell, etc. 7. In animal studies, marginal vitamin A intakes lead to a variety of “fetal malformations” including defects in kidneys, lungs, and eyes. 8. The human studies we have indicate that low vitamin A intakes are linked to low birth weight, premature birth, poor kidney, eye, and lung development or maturation; in developing countries it manifests as blindness and increased infant mortality. Very large doses are safely given to newborns in these countries. 9. Governmental and medical recommendations are fairly similar across countries: about 2500 IU per day for pregnant women, only about 10% more than for a non-pregnant women. 10. There are public health agencies that continue to recommend that pregnant women consume liver, mainly for its iron content to prevent or treat anemia. Not well know is the fact that vitamin A, B6, and B12 in liver are also required for the production of red blood cells. 11. Over half of American women ages 18-30 do not meet vitamin A requirements from diet, using an EAR of 1670 IU, not the RDA of 2570 IU. There is evidence that lower-income women have intakes low enough to warrant serious concern. 12. The FDA’s daily value for pregnant women is 8,000 IU, used for supplement and food labeling (and based on the RDA’s established in 1968, now replaced). This was also considered a safe intake according to the CDC’s scientists. 13. There is a widespread and unfounded fear among obstetricians that vitamin A is to be avoided; they prescribe or recommend prenatal vitamins very low in vitamin A which are largely what pharmaceutical companies make. 14. It is thought that all babies are inherently born with low vitamin A stores, but it has been shown that in developing countries stores are even lower, indicating the mother’s intake does affect the stores. Correlations between mothers’ vitamin A levels and fetal levels/growth have been shown. 15. Breast milk is affected by the vitamin A status of the mother; colostrum can contain 10 times more vitamin A than more mature breast milk. 16. It is not easy to assess the vitamin A status of an individual; serum retinol does not go to low levels until the liver is virtually depleted. Methods of assessment are discussed in the article. There are tell-tale physical signs, such as hyperkeratosis, night blindness, and acne. 17. Iron and zinc play roles in vitamin A metabolism. However, routine iron supplementation may not be advised depending on the iron stores of the women as there is a risk for an increase of gestational diabetes. 18. Very importantly – an excessive intake of vitamin D from supplements is potentially dangerous for a pregnant woman because of the need to balance with vitamin A and K2. It is not unusual for an OBGYN to recommend 5000 IU of vitamin D per day, in addition to the amount in the prenatal. 19. Vitamin A intakes of 10,000 IU per day from food are generally agreed to be safe; however, it a women is anticipating pregnancy and wishes to avoid this intake, she can build up her stores pre-conceptually. The consensus is any risk of birth defects exists between day 15 and day 60 following conception. 20. Traditional societies consumed foods rich in vitamin A including fish eyes and organ meats, and valued these as special foods for couples wanting to have children.

This is a subject that gets a lot of medical attention but scant nutritional attention. I hope to shed some light on a situation that you may be facing, whether you are trying to conceive or you want to enjoy your sex life more. Our bodies produce a wonderfully lubricating mucous in a variety of places; it serves to keep our eyes, skin, nasal passages, lungs, and digestive tracts from getting dried out, and keeps germs for gaining a foothold into these surfaces, surfaces that are continuously exposed to the outside world. Oh, and just as importantly, it keeps our “reproductive canal” nice and moist. Healthy mucous clearly is something we want to encourage for all of these important reasons. If we want to get pregnant, we especially want to optimize the quality and quantity of cervical mucous (some call it “fluid”), fundamental to supporting our natural fertility. If we are dealing with menopausal vaginal dryness, we don’t want to make it worse because we are not giving our bodies what we need to produce as much mucous as our hormones allow. Proper nutrition, adequate hydration, and balanced hormones all play a part in ensuring we are optimizing mucous production. As a nutritionist, I want to tell you about a vitamin most of us don’t get enough of that is absolutely essential for mucous production. That is vitamin A. No, not vitamin A from carrots and sweet potatoes. While those are healthy foods I love and encourage my clients to eat, for most women, they won’t help reverse things like dry eyes, dry bumpy skin, or a dry cervix or vagina. To address that, real vitamin A is best. The kind you get from liver, cod liver oil, and deep orange egg yolks (and fish eyes if you are so inclined!). These foods long removed from our menus are the very fertility foods that un-modernized societies valued for healthy reproductive function. If you feel the thought of eating liver is too much to consider, try this recipe for chicken liver pate – http://cooking.nytimes.com/recipes/1012954-creamy-chicken-liver-pate , you may actually like it and best of all, it is super healthy for you and your mucous. (Interestingly, in my research for this article I came across a patent for the use retinoic acid, a form of vitamin A, inter-vaginally to effectively address postmenopausal dryness. I also learned there was a clinical study which showed a beneficial effect on the bacterial vaginosis among pregnant women, thought to be due to enhancement of the vaginal surface barrier – Christian P, et al. Maternal vitamin A and beta-carotene supplementation and risk of bacterial vaginosis…Am J Clin Nutr 2011;6: 1643.)

I typically recommend for my expectant couples one of a few curated prenatal vitamins, (either from Seeking Health, Xymogen, or Brain Smart MD) available at https://us.fullscript.com/welcome/pschoenfeld . One of these may be a good match for you and your baby’s needs, but a fully nourishing diet is always the best foundation. OBGYNs typically suggest over-the-counter prenatals, advising to make sure they contain folic acid. Most OTC prenatal vitamins also contain iron, some as much as 45 mg in a single tablet or capsule. This aligns with the CDC and the American College of Obstetricians and Gynecologists which both recommend universal consumption of prenatal supplements containing iron to meet pregnancy needs and to prevent anemia. A woman has an increased need for iron during pregnancy as her blood volume expands and the demands of her growing baby and placenta increase. According to WEBMD.com, she needs 27 mg per day during pregnancy, and 9 mg during lactation; mirroring the Institute of Medicine recommendations. A large percentage of women have iron deficiency during their reproductive years. During pregnancy, the likelihood of iron deficiency increases with each trimester, 7% of women in the first, 14% in the second, and 30% in the third trimester are diagnosed with iron deficiency or anemia (1). So it would seem to make good sense to take a prenatal vitamin with iron during pregnancy. But let’s take a closer look. What are the risks of iron deficiency during pregnancy? Supplemental iron is considered relatively safe, and acording to the National Library of Medicine at NIH:

PCOS – Lowering Insulin Levels with Diet You may be expecting me to discuss lowering your carb intake – and thinking, so tell me something I don’t know. Please keep reading on, this is not the same old advice. While excess refined carbs are clearly a problem, most women with PCOS will reduce “white” foods and sugar as their first dietary change; and many see results, especially with modest weight loss. But is there more you can do? Yes, and you may find it an easy change to make. It is simply cooking your food at lower temperatures with plenty of moisture. I advise most of my patients not to grill, and if they do so, to limit how dark they cook their food, and ideally marinating with acid-marinade for at least a few hours before grilling. Ditto for eating fried foods – I recommend they be eaten minimally if at all, especially considering the highly-damaged fats they are fried in. This is to limit the consumption of chemical by-products when protein and/or carbohydrates are heated to temperatures in excess of 400 degrees. Now we are learning that any type of dry, heat cooking – even sauté – is associated with increased fasting insulin levels in healthy adults. In fact, after a year of modifying their diets to a low “AGE”, or advanced glycation product containing diet, the individuals who used low-temp cooking techniques had more than a one-third reduction in fasting insulin levels compared to those who used high-temp cooking methods. You may know that increased insulin levels are linked to an increased output of testosterone from the ovaries in women with PCOS. So while the participants in this study did not have PCOS, it is a fair assumption that a low AGE, or low-temp cooked diet, could be helpful to you if you have been diagnosed with PCOS. Another benefit is the reduction of markers of inflammation, such as hsCRP, which are often elevated in PCOS. While boiled or poached food may not be as tasty, the use of spices and low-sugar sauces can help you adjust to the change. Some suggestions would be to eat soft or hard-boiled eggs instead of fried, beef stew instead of grilled steak, poached fish instead of grilled, baked meatballs instead of fried (keep oven around 300 degrees and don’t overbrown), raw versus roasted nuts, and raw milk cheese instead of cheese made with pasteurized milk. Vegetables can be lightly steamed and will maintain a good crunch such as with a stir-fry. Sorry, you will have to forgo toasting your bread, even your whole grain bread; similarly, most dry cereals are moderately high in AGEs, stick to oatmeal. And baked potatoes in the skin are clearly better than oven-roasted potatoes even when using healthy oils like ghee or olive oil. The key is to keep food from getting darker in color as you cook it. If you are looking for more advice on how to manage your PCOS, please give me a call and take advantage of my free 10-minute consult to see if I am a good fit for your needs. There are many nutritional options including some very helpful supplements your doctor may not be aware of. I have seen good results in women of all ages – less unwanted hair, less acne, weight loss, and restoration of regular cycles – by following some relatively simple changes.

I just completed an article soon to be published in a popular nutrition journal which sheds some light on the question posed above. The answer might seem yes, of course, that goes without saying. However, in reality, it is not as simple as some might think. Vitamin D is a versatile nutrient, and like all vitamins, we can’t live without out it. But unlike all of the other vitamins, it does not have to come from our food, we can get all we require from the sun. But since most of us don’t spend much time in the sun, or use sunscreen when we are outside, dietary sources are important. Many of my patients are already taking vitamin D when at our first meeting. Some have had blood testing done to check their vitamin D levels. While these are generally good practices, I take a slightly different approach to vitamin D supplementation – I make sure that vitamin D is not the only vitamin that needs to be supplemented. Vitamin D works in concert with vitamins A and K, vitamins that many women also don’t get enough of for a number of reasons. What can happen if you take vitamin D on its own? Nothing terrible in most cases, but if too much vitamin D is taken for too long a period of time, there is a potential for some calcium deposits to occur in soft tissues like the kidneys. As soon as this article is published, I am going to post the link for those who want a more complete understanding of what needs to be considered when taking vitamin D.






